obesity
Nutrisystem is a smarter weight-loss program that users enjoy.
Research finds that our sense of self can be manipulated by certain smells and sounds.
The human body is endlessly fascinating.
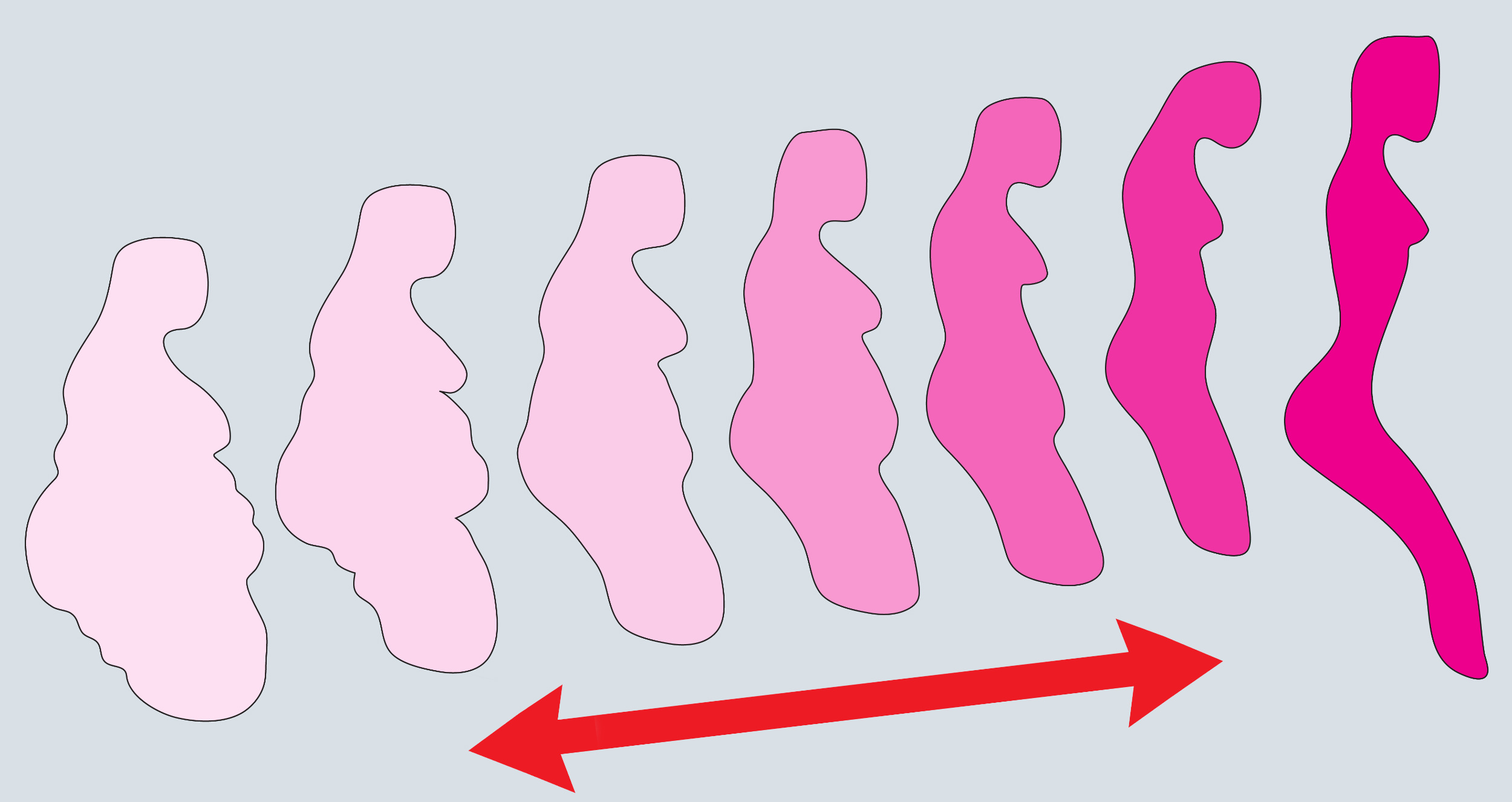
Is focusing solely on body mass index the best way for doctor to frame obesity?
The study was only conducted with already healthy men, however.
Johns Hopkins University professor Susan Carnell explains the neuroscience behind eating out of boredom (and how to stop).
Once again, sugar-rich processed foods are shown to increase the likelihood of anxiety.
A new research article states that the obesity epidemic is affecting more than just waistlines.
Unhealthy diets cause the part of your brain responsible for appetite to become inflamed, encouraging further eating and obesity.
Bill Maher called for fat shaming last week. His argument makes sense.
The reason one diet does not suit all may be found in our guts.
A new study found a positive association between sugary drinks and cancer.
A new study has bad news for those who binge watch TV.
The results show how diets high in saturated fat can cause fatty acids to build up in the hypothalamus, disrupting its normal functioning.
Turns out a little obsession is a good thing.
Junk food causes weight gain, but it’s not just about the calories.
A new research letter points to another reason for childhood obesity.
Two new studies say yes. Unfortunately, each claims a different time.
The calorie is the basic unit of measure of food — and it might be off.
Vitamins do work — when eaten in whole foods, not pills.
Education shouldn’t just be about preparing us for the workforce. It should prepare us for life.
Good bacteria are our friends. We need to protect them.
▸
3 min
—
with
As plant-based burgers get tastier and the health benefits become clearer, we might soon see more carnivores go meatless.
A new study explores how certain personality traits affect individuals’ attitudes on obesity in others.
Turns out the more we desire a food, the more we have to consume to feel satiated.
A new study out of the University of Tennessee, Knoxville traces a disturbing correlation.
It isn’t mind over matter as much as mind properly working with matter.