cancer
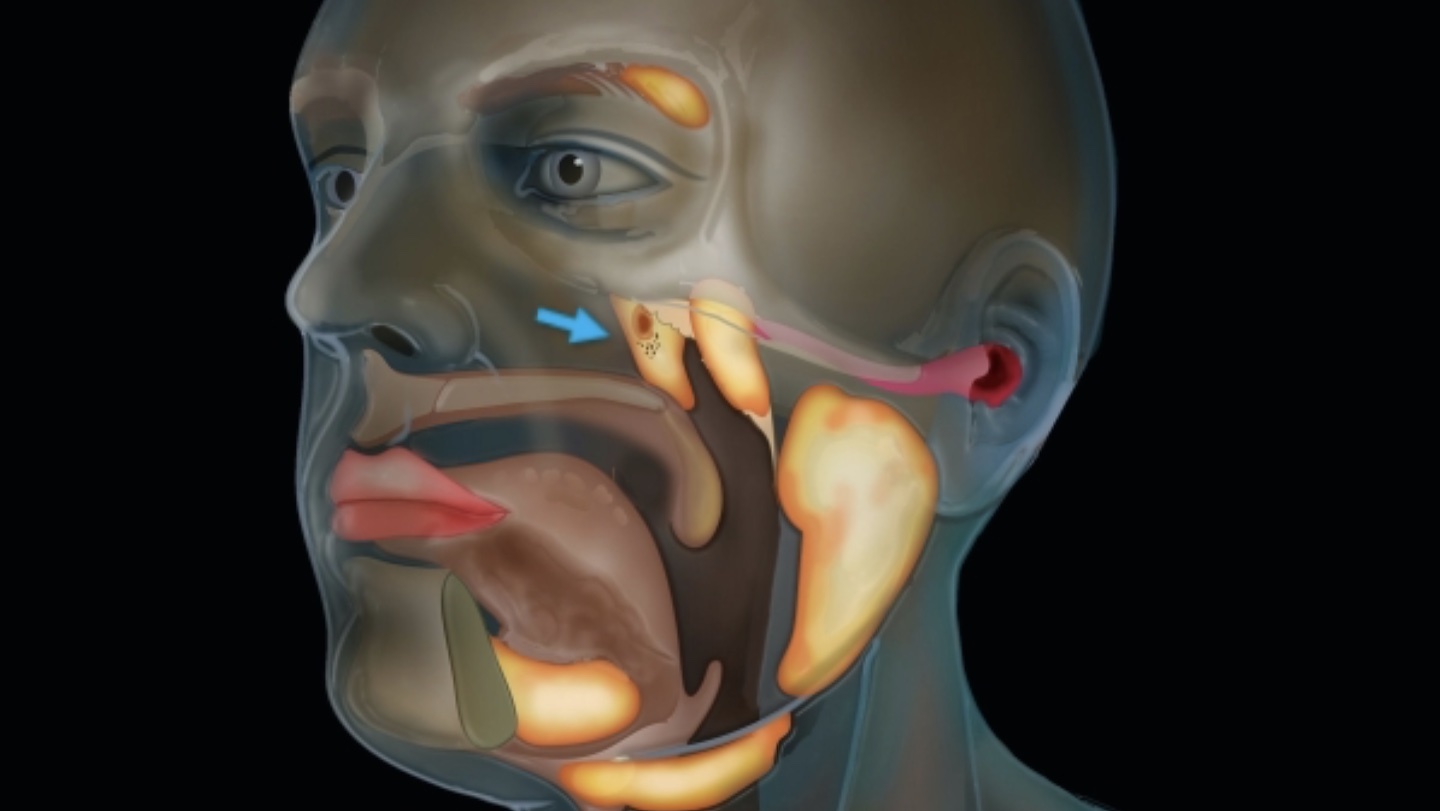
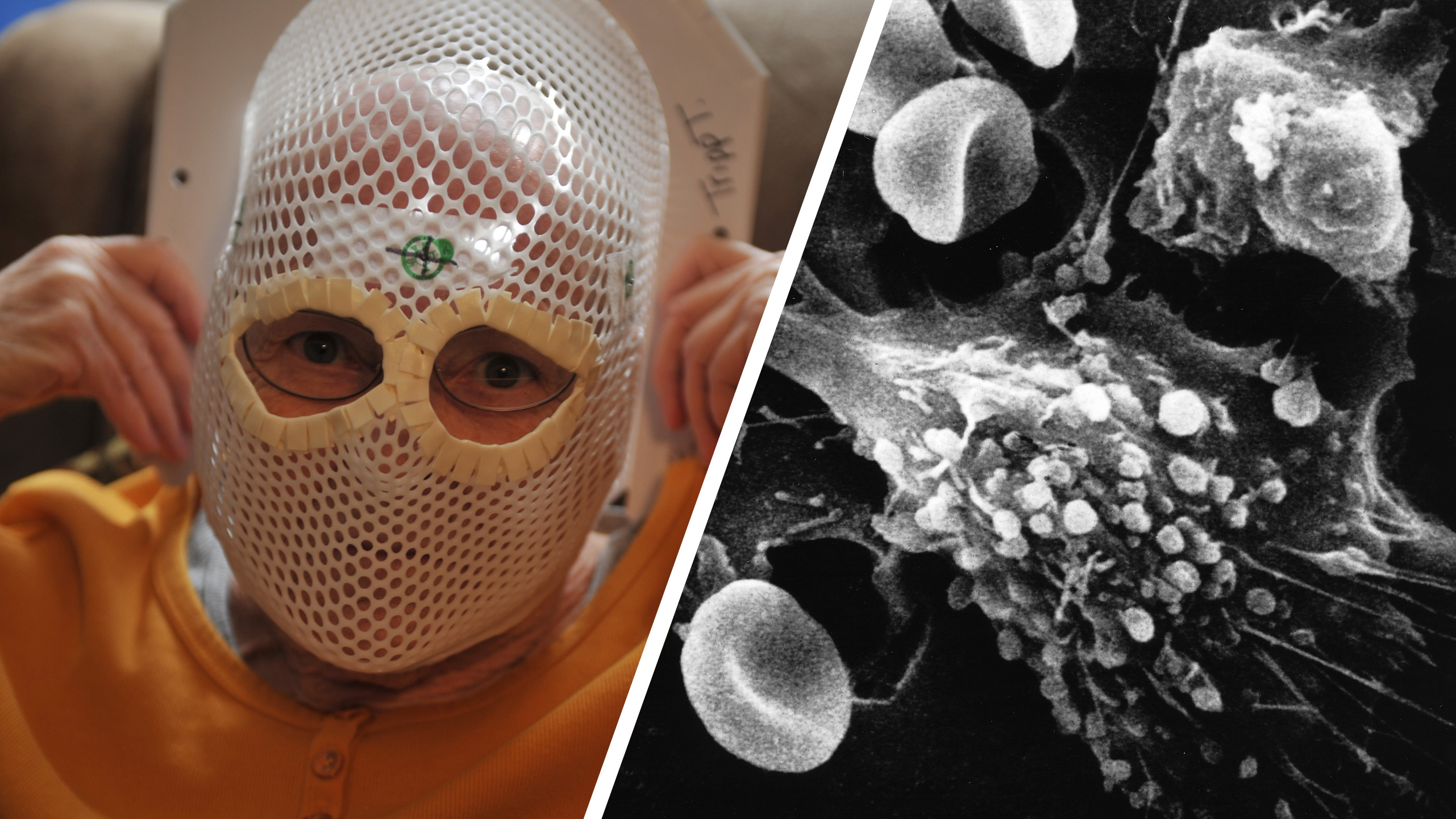
The new brain tumor treatment targets a cancer that kills 75% of patients within a year.
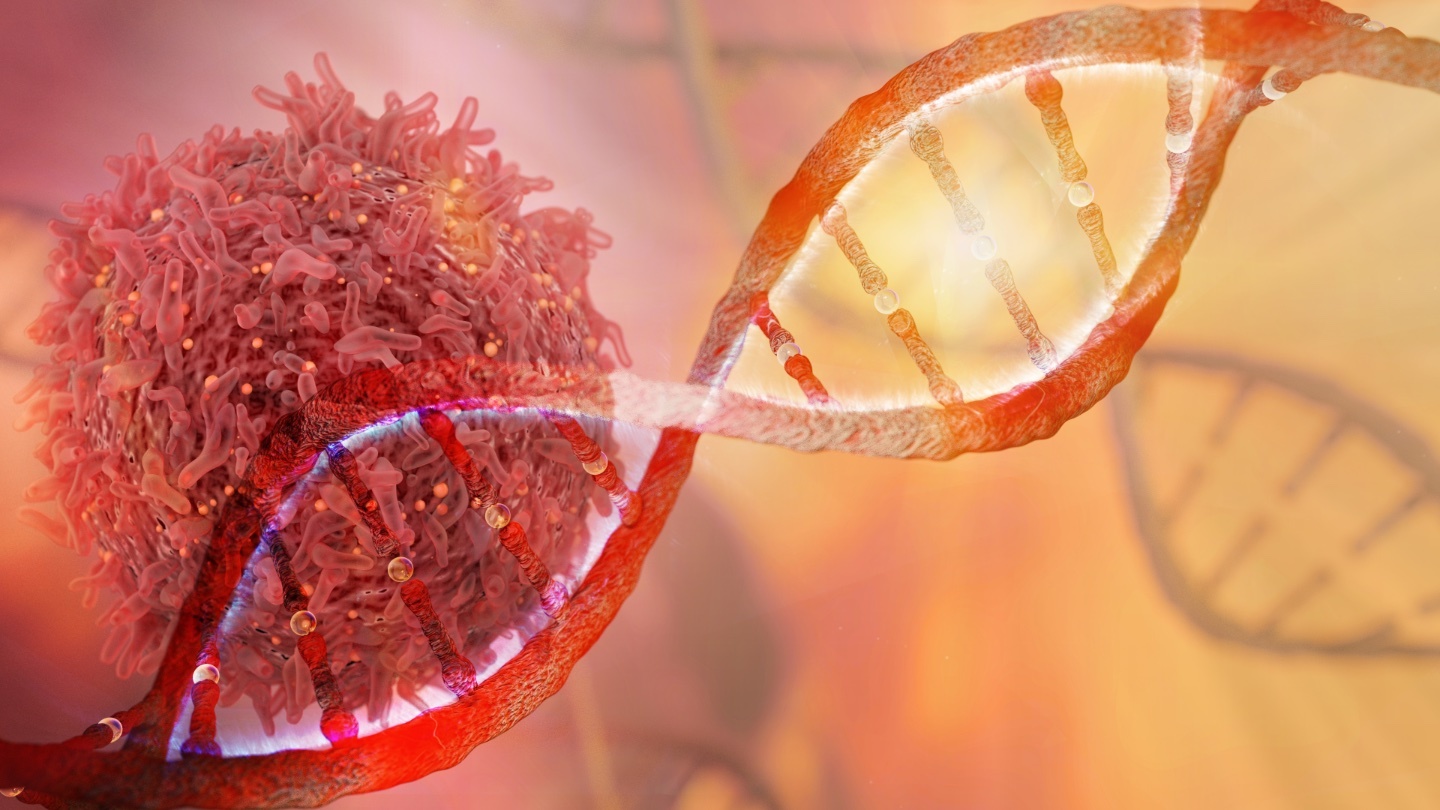
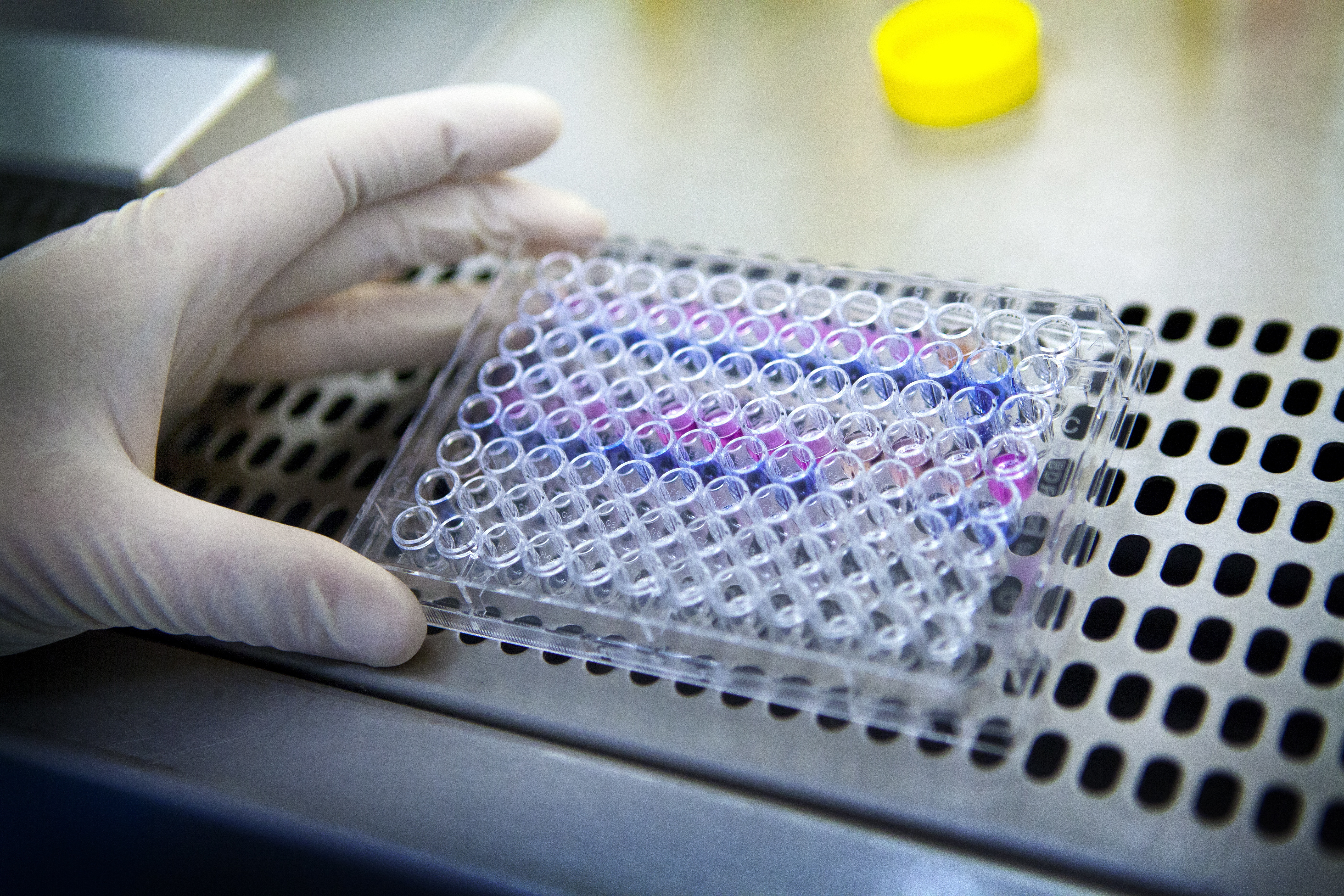
Using image analysis tools developed for astronomy, researchers are predicting cancer therapy responses.
As the American population grows, fewer people will die of cancer.
Engineered immune cells have prevented Type 1 diabetes in mice.
A study says nature’s candy can be a valuable supplement to sunblock.
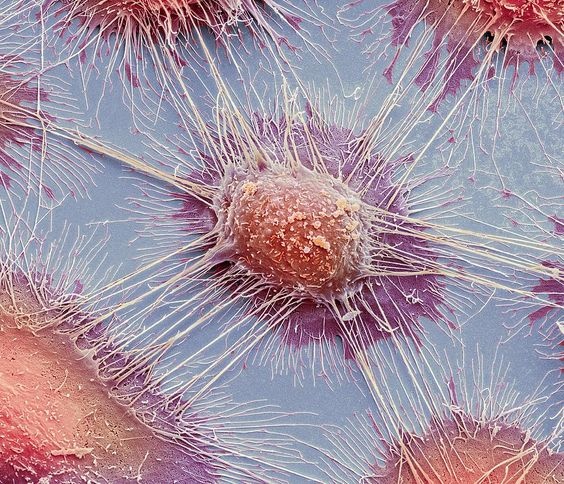
Researchers discover that cancer cells go into hibernation to avoid chemotherapy effects.
What lies in store for humanity? Theoretical physicist Michio Kaku explains how different life will be for your descendants—and maybe your future self, if the timing works out.
▸
15 min
—
with
New cancer-scanning technology reveals a previously unknown detail of human anatomy.
Researchers from the University of Toronto published a new map of cancer cells’ genetic defenses against treatment.
A large-scale study from King’s College London explores the link between genetics and sun-seeking behaviors.
An active component of honeybee venom rapidly killed two particularly aggressive forms of breast cancer in a laboratory study.
Despite Boseman’s young age, this cancer is increasingly common in people under 50.
Just how close are we to setting up camp on another planet? It’s complicated.
▸
17 min
—
with
A recent analysis of a 76-million-year-old Centrosaurus apertus fibula confirmed that dinosaurs suffered from cancer, too.
Scientifically, it’s referred to as ‘cancer-related cognitive impairment’ or ‘chemotherapy-related cognitive dysfunction’.
One study says reduce red meat consumption; another says enjoy. Which should we believe?
Scientists figured out how a certain treatment for skin cancer gives some patients a visual “superpower.”
In 2018, cancer drugs earned the pharmaceutical industry $123.8 billion. Soon, they’ll be worth billions more.
Numerous drugs designed to treat diabetes, arthritis, and other conditions may actually have secret anti-cancer properties as well.
A 2020 space mission wants to use zero gravity to disable some of the hardest cancers to fight.
Embracing signs of age might be the road to a longer life after all.
Your microbiome begins in your mouth. Why don’t we look there more often?
The possibility of an easy, non-invasive detection method arises.
The team seems to have found a way to extend animal lifespan without genetic modification.
A single typo in the “dark matter” of the genome drives multiple types of cancer.
A new immunotherapy treatment is showing positive signs in early-stage clinical trials.
How do you develop the next big idea? You pull together people who are both curious and passionate.
▸
4 min
—
with
Has misinformation clouded our understanding of the anti-aging power of hormones?
▸
5 min
—
with
Even before publication, health agencies were asking the journal not to publish the research.
The large-scale study got it right for 83 percent of participants. Would you take the blood test?