- A blood test that spots breast cancer five years ahead of clinical signs could give new meaning to “early detection.”
- Auto-antibodies for tumor antigens predict the presence of the disease.
- Researchers say the blood test could be clinic-ready in 4-5 years.
Researchers from the University of Nottingham have developed a method of blood screening they believe could ultimately lead to the detection of breast cancer five years before clinical indicators appear. Such extremely early detection would presumably offer patients and their doctors an unprecedented head start at preventing the disease’s progression. The availability of such an advanced warning would be a potent addition to the growing arsenal of weapons against breast cancer that include a breast-cancer vaccine.
Antigens and their auto-antibodies
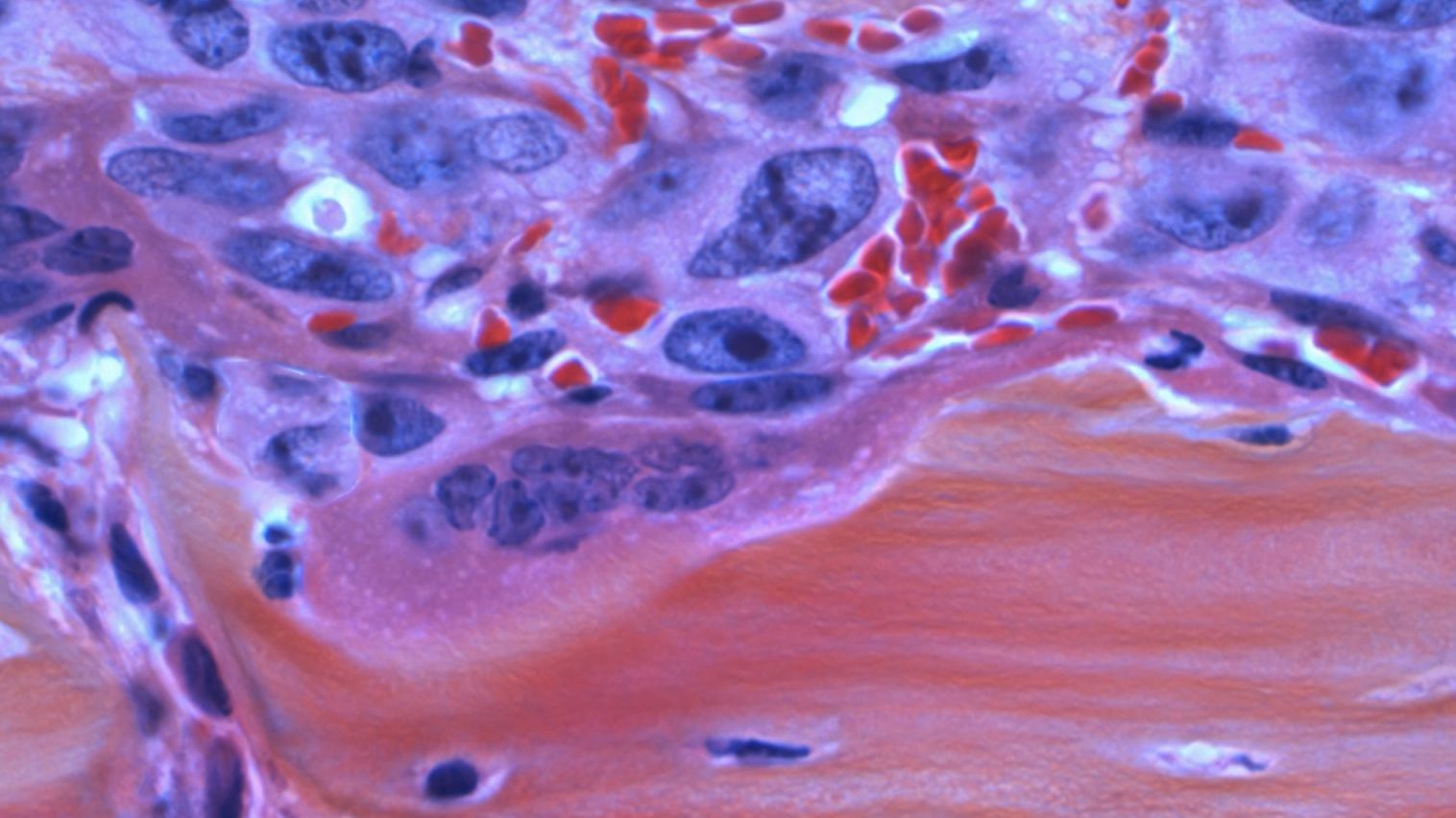
Antigens are substances produced by cells, including tumor cells. When an antigen comes into contact with other cells in the body, the immune system generates an antibody optimized specifically for that antigen called “auto-antibodies.”
The team from Nottingham has found that the presence of tumor-associated antigens (TAAs) constitutes a reliable indicator of cancer. Likewise, the presence of an antigen’s auto-antibody is a good indicator that the antigen, and thus a tumor, is present.
The researchers developed blood panels against which blood can be screened using protein microarray for auto-antibodies linked to TAAs associated with breast cancer tumors. The team was able to screen for 40 such antibodies overall, as well as 27 not associated with the disease, with each panel targeted to a subset of those.

Image source: Victor Moussa/Shutterstock
The experiments
The researchers from the Centre of Excellence for Autoimmunity in Cancer (CEAC) group at Nottingham’s School of Medicine took blood samples from 90 breast cancer patients shortly after diagnosis, and from a control group of 90 volunteers not afflicted with the disease.
According to Daniyah Alfattani, one of the researchers, “The results of our study showed that breast cancer does induce auto-antibodies against panels of specific tumor-associated antigens. We were able to detect cancer with reasonable accuracy by identifying these autoantibodies in the blood.”
The team focused on three panels: One with five TAAs, one with seven, and one with nine. The larger the panel, the more accurate the testing, as it turned out.
- With the panel of five TAAs, breast cancer was detected in 29% of the samples from cancer patients, while 84% of the control samples were positively identified as being without cancer.
- With seven TAAs, the cancer-detection rate rose to 35%, while the findings of no disease in the control group went down slightly to 79%.
- A nine-TAA panel was similar, correctly detecting cancer in 37% of cancer patients, and its absence verified it in 79% of the control group.

Image source: Simon Annable/Shutterstock
Moving forward
While accurate cancer detection in roughly 30% of patients isn’t anywhere near good enough for widespread use as a diagnostic tool, the researchers are nonetheless upbeat about the results. “We need to develop and further validate this test,” says Alfattani. “However, these results are encouraging and indicate that it’s possible to detect a signal for early breast cancer. Once we have improved the accuracy of the test, then it opens the possibility of using a simple blood test to improve early detection of the disease.”
Further study is currently underway with 800 patients being tested using a panel of nine TAAs, and the researchers expect to see greater accuracy in this larger cohort.
If there’s a chance of substantially improving accuracy in this approach to early detection, the benefits would be obvious. Says Alfattani, “A blood test for early breast cancer detection would be cost effective, which would be of particular value in low- and middle-income countries. It would also be an easier screening method to implement compared to current methods, such as mammography.”
The researchers estimate that with full funding, a clinic-ready version of the test could be developed in four to five years.
The study was presented at the 2019 NCRI Cancer Conference in Glasgow, and NCRI CEO Iain Frame is impressed. “Early diagnosis using simple, non-invasive ways of detecting the first signs of cancer is a key strategic priority for NCRI and something we’d all like to see working in practice. The results from this pilot study for a blood test to detect early breast cancer are promising and build on this research group’s expertise in other cancers, such as lung cancer. It’s obviously early days but we look forward to seeing the results from the larger group of patients that are now being investigated.”