10 new things we’ve learned about cancer

- Cancer is a leading cause of death among Americans, second only to heart disease.
- Researchers are unearthing cancer’s genetic secrets and, with it, potential new treatments.
- Their efforts have seen the cancer death rate for men, women, and children fall year after year between 1999 and 2016.
The 21st century has been, and will continue to be, shaped by cancer. Although heart disease remains the United States’ number one killer, cancer is quickly closing the gap and may soon surpass it. Some oncologists claim a cure is five, 10, certainly no more than 20 years away. Others aren’t so sure because, in a way, cancer is the price we pay for evolutionary success.
“It is no coincidence that the very genes that allow our embryos to grow — our hands to grow, our feet to grow — if you mutate them in inappropriate contexts, [they] will ultimately release the disease that kills us,” said oncologist Siddhartha Mukherjee, who dubbed cancer the Emperor of All Maladies, also the title of his Pulitzer Prize-winning book.
Whether for five years or forever, cancer won’t be going anywhere any time soon. Yet, the more doctors and scientists discover about it, the better we can learn to live with it.
A love-hate relationship: Cancer and antioxidants
Contrary to what many believe, cancer enjoys a nutrient-rich diet as much as the next cell because it helps it grow, even those legendary antioxidants.
In two independent studies published in Cell, Swedish and American research teams found that lung cancer utilizes antioxidants to activate a protein called BACH1. This protein stimulates the cancer cells to metabolize glucose and accelerate metastasis. Even without a ready supply of dietary antioxidants available, the tumor would simply produce its own.
Professor Martin Bergo, who led the Swedish study, hopes this research will help develop new treatments. “We now have important new information on lung cancer metastasis, making it possible for us to develop new treatments, such as ones based on inhibiting BACH1,” he said in a release.
Does this mean you should abstain from antioxidant-rich foods? Not at all. Antioxidants do neutralize the free radicals that cause oxidative stress on cells. Preventing such cell damage can help prevent cancer.
However, it’s best to avoid antioxidant supplements unless prescribed by a doctor. As reported by the National Cancer Institute, of nine randomized-controlled clinical trials, none provided evidence that such supplements lower cancer risks. A few even found that beta-carotene supplements increased the risk of lung cancer so severely that the trials had to be ended prematurely.
Get your antioxidants from fruits, veggies, and beans instead. Research suggests that these antioxidants work in combination with additional molecules found in the whole foods. It’s this tag-team effect that ultimately give antioxidants their salubrious power.
Cancer costs (in more ways than one)
It goes without saying that cancer is costly. The physical strain of treatment. The potential loss of life, whether one’s own or the life of a loved one. And even if one survives, there’s the emotional cost of the ordeal.
But the toll imposed by cancer is more than physical or psychological. A study released last year found “that 42 percent of patients deplete their life savings during the first two years of treatment.” Of the 9.5 million newly diagnosed cancer patients surveyed, the study calculated average losses at $92,098.
Its authors dubbed the effect “financial toxicity” and concluded: “As large financial burdens have been found to adversely affect access to care and outcomes, the active development of approaches to mitigate these effects among already vulnerable groups remains of key importance.”

A recent study found a positive association between a daily sugary drink and an increased risk of cancer.
Cancer’s sweet tooth
Researchers asked more than 100,000 people to complete surveys looking at their usual consumption of 3,300 foods and beverages. The results? A positive association between daily consumption of a sugary beverage and an increased risk of cancer. The sugary drinks not only included soda but also 100 percent fruit juice and artificially sweetened drinks.
“These data support the relevance of existing nutritional recommendations to limit sugary drink consumption, including 100% fruit juice, as well as policy actions, such as taxation and marketing restrictions targeting sugary drinks, which might potentially contribute to the reduction of cancer incidence,” the researchers stated in a release.
Don’t go trashing the OJ just yet, though. As an observational study, the data could not establish a cause-effect relationship, and the researchers note the results are only preliminary. Additionally, the results hinge on the memories of the participants. (What exactly did you eat for breakfast the Monday before last?)
But the study helps stress the American Institute for Cancer Research’s (AICR) suggestion to limit sugary beverages. Try to remove soda from your diet. Drink 100 percent fruit juices with no added sugar sparingly. And of course, enjoy an active, healthy lifestyle.

Cancer on the grill
It’s a summer tradition to throw some meat on the grill alongside a good beer. But grilled meats hide a few furtive carcinogens: polycyclic aromatic hydrocarbons and heterocyclic aromatic amines.
The hydrocarbons are carried in the smoke after fat burns on the flame, while the heterocyclic amines form when sugars, amino acids, and creatine react at high heats. Neither has been proven to cause cancer, but they are known mutagens that can damage DNA after being metabolized.
“Research shows that diets high in red and processed meat increase risk for colon cancer,” said Alice Bender, AIRC Senior Director of Nutrition Programs. “And grilling meat, red or white, at high temperatures forms potent cancer-causing substances.”
Like sugary drinks, however, you don’t have to forever hang up your “Kiss the Cook” apron. The institute has several suggestions for safe summer grilling, such as limiting red meat, marinating foods beforehand, keeping a low flame, and throwing more vegetables into the mix.
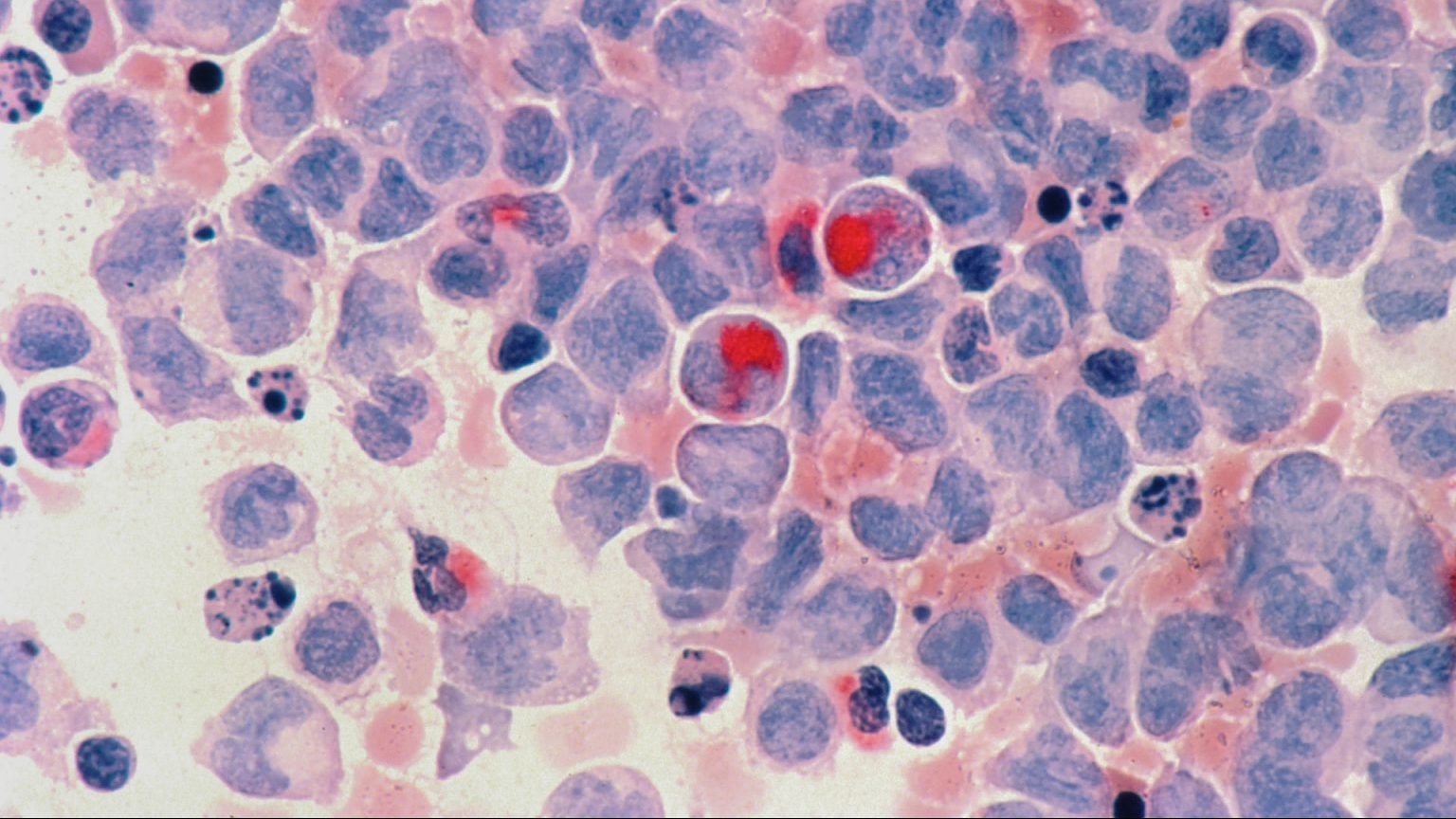
A unified theory of leukemia
Acute lymphoblastic leukemia (ALL) afflicts about one in 2,000 children, and Mel Greaves, at the Institute of Cancer Research, London, believes he’s found the cause. Researching 30 years of data and medical literature on childhood leukemia, he argues the “delayed infection” is the culprit.
According to this theory, children develop a pre-leukemia mutation in utero. The mutation remains inert until later in life when the child encounters a common infection. The microbes then trigger secondary genetic changes that led to overt leukemia.
Does this mean children are safe only in cleanrooms? Strike that, reverse it. Greaves believes exposure to germs in the first year of life is proactive. It trains the immune system to deal with pathogens, therefore preventing the secondary mutation from triggering.
“Childhood ALL can be viewed as a paradoxical consequence of progress in modern societies, where behavioral changes have restrained early microbial exposure,” Greaves writes. “This engenders an evolutionary mismatch between historical adaptations of the immune system and contemporary lifestyles. Childhood ALL may be a preventable cancer.”
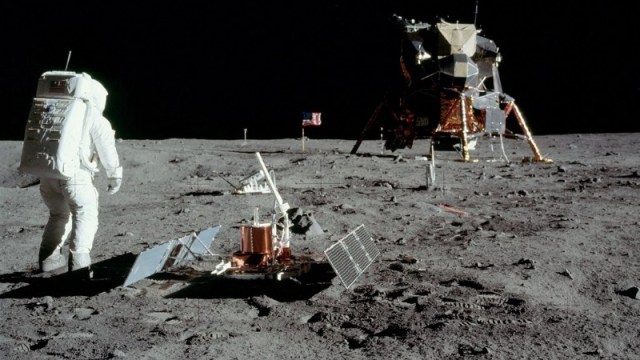
The future of cancer treatment is genetic
A major stride toward our understanding of cancer came with the Human Genome Project. Why? At its core, cancer is a genetic disease.
Our ability to sequence and read cancerous genomes will be a major step toward cancer treatments. As Eric Green, director of the National Human Genome Research Institute, told Big Think:
“[The] standard of care for many types of cancer is going to be: Get that tumor, read out its DNA, sequence its genome and based on what you’ve seen what’s wrong with that tumor — not by looking at it under a microscope only or by looking at it in a sort of a gross fashion but actually looking inside its blueprint — you will be able to have a much better way of deciding what types of treatments to pursue and have a much better idea about what’s wrong in that kind of tumor.”

An airman receives a vaccine. Could the future of cancer treatment be as easy as a shot?
A future treatment? The “cancer vaccine”
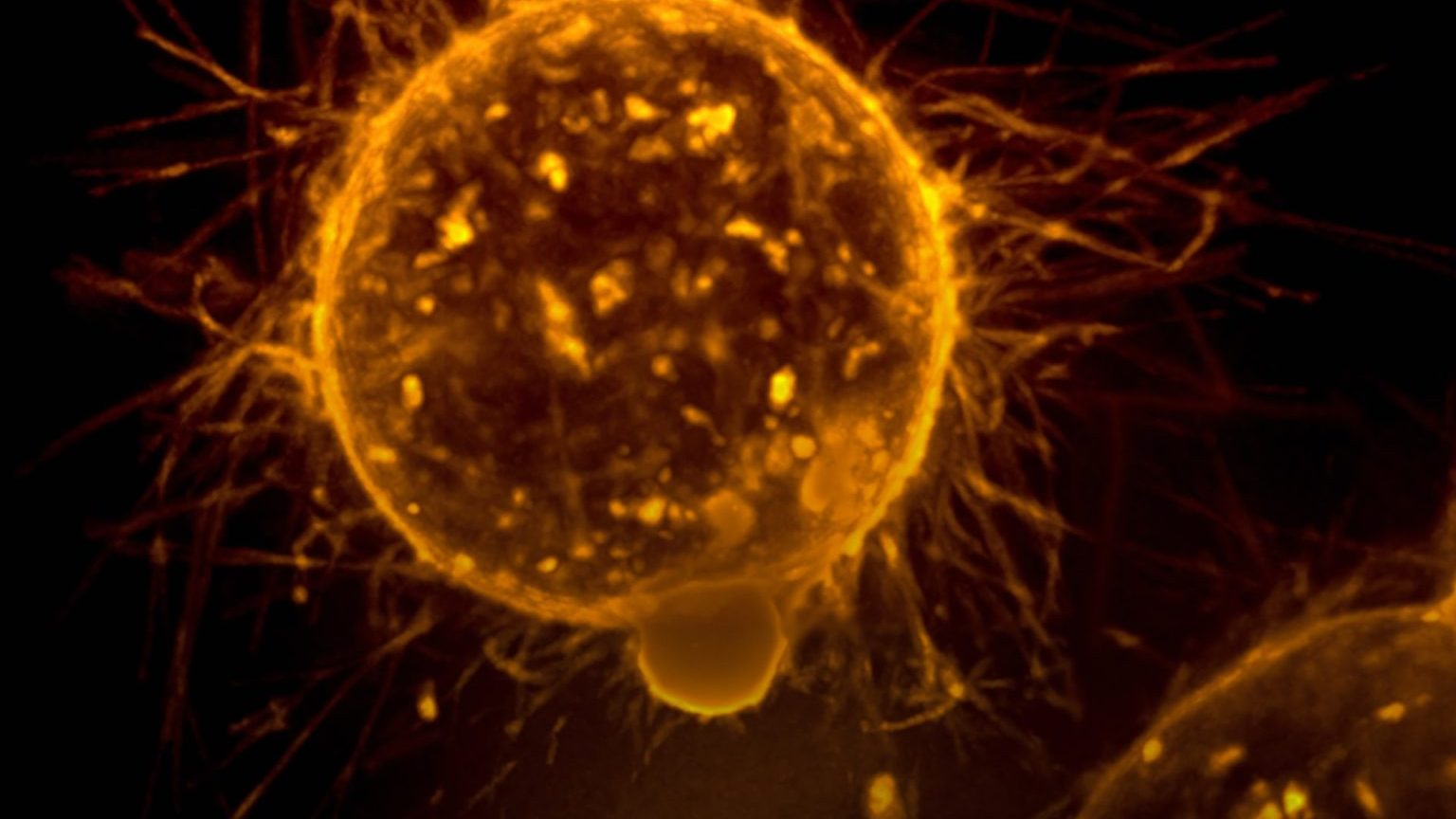
Rather than using chemotherapy to combat cancer with the subtlety of an atomic bomb, immunotherapies aim to uncloak cancer cells, so the body’s immune system can go on the offensive
One example of an immunotherapeutic approach is the so-called “cancer vaccine.” During its clinical trial, 11 patients had a tumor injected with a steroid to bolster the site’s dendritic cells — immune system cells that specialize in processing antigens.
Following a light dose of radiation and a stimulant, the patients’ dendritic cells directed T-cells to attack the cancer cells. Once the T-cells could recognize the tumor, they became able to locate cancer cells throughout the body.
Of the 11 patients, three saw their cancer go into regression or remission. Six others had their cancer stymied for at least three months.
“It’s really promising, and the fact you get not only responses in treated areas, but areas outside the field [of treatment with radiation] is really significant,” Dr. Silvia Formenti, chairwoman of radiation oncology at Weill Cornell Medicine and New York Presbyterian, told CNBC. (Dr. Formenti was not involved in the study.)
Turning tumors into fat
A deadly tool in cancer’s arsenal is cell plasticity, a cell’s ability to alter its physiological characteristics. It is one of the reasons cancers can metastasize throughout the body, and it helps the disease resist treatments.
Researchers at the University of Basel, Switzerland, have hijacked this ability and turned it against cancer. Using a drug therapy that combined an anti-diabetic drug and MEK inhibitors, they attacked cancer cells and turned them into adipocytes (a.k.a. fat cells).
While this did not remove the tumor, it did make the cells post-miotic, meaning they could no longer divide. This inhibited the cancer’s ability to spread.
“In future, this innovative therapeutic approach could be used in combination with conventional chemotherapy to suppress both primary tumor growth and the formation of deadly metastases,” senior study author Gerhard Christofori told Medical News Today.

An image of the E. coli bacteria. Will these become the next breakthrough in cancer therapies?
Cancer-killing bacteria
Another advancement in cancer treatment is synthetic biology, a field in which scientists use the principals of engineering to redesign biological systems. In one example, researchers genetically programmed a non-pathogenic E. coli strain to attack tumors in lab mice.
Once injected, the rewired bacteria took refuge in the tumor, where they self-destructed. These dead bacteria leaked from the tumor, and thanks to encoded nanobodies, drew the attention of T-cells which devoured the bacteria and tumor alike.
Of course, lab tests in mice do not guarantee a successful transition to human patients, but it remains a promising avenue for treatment.
“At some point in the future, we will use programmable bacteria for treatment,” Michael Dougan, an immunologist at Massachusetts General Hospital, told the New York Times. “I think there’s just too much potential.”
A new attitude toward cancer
Medical professionals originally viewed cancer as a disease to be destroyed with extreme prejudice; the treatment was only better than the disease because the disease ended in death.
But as David Agus, professor of medicine and engineering at USC, told us, there are better ways to approach cancer:
“Well, to me cancer is a verb and not a noun. You’re cancering, it’s something the body does and not that the body gets. And so that philosophy needs a very different way of approaching disease, and it means changing the system in addition to trying to target the cancer.”
One way is to approach treatment holistically. Agus points to a trial that gave premenopausal women with breast cancer a bone-building drug. The drug didn’t target the cancer, yet it reduced recurrence by 40 percent because breast cancer metastasizes in bone.
Another method is psychosocial oncology. In this relatively new field, the practitioners’ goal is to enhance the quality of life for cancer patients through mental health care as a part of physical care.

Cancer death rates in the United States by cancer type, male and female, age standardized.
Living with cancer
Scientists have learned a lot about cancer, but there remains much we don’t know. Does that mean we should despair for the future? Quite the contrary. Thanks to the knowledge accumulated by scientists, we have much to be hopeful for.
Headlines are correct that the total number of new cancer cases and deaths continue to increase. However, the rates of cancer diagnoses and death have declined year after year. This is because absolute numbers don’t account for metrics like population growth and increased life expectancy. In fact, the Annual Report to the Nation on the Status of Cancer found that the cancer death rate for men, women, and children fell year after year between 1999 and 2016, as did cancer incident rates.
“Death in old age is inevitable. The job of science is to prevent unanticipated deaths in unanticipated times. I find that is a perfectly reasonable goal,” said Mukerjee. “If you’re saying to me that we will have a more profound, more proximal reconciliation with cancer in the next few decades, I think the answer is absolutely yes.”
We may not be able to eradicate cancer as we did with diseases like smallpox and polio. But we’re learning how to live with it more and more every day.