Statins aren’t overprescribed. Maybe we should put them in our drinking water
- Cholesterol-lowering statins are prescribed to 200 million people worldwide, leading some to question whether their ubiquity is called for.
- Reviewing the available evidence dispels most concerns. Statins are amazingly effective at reducing death from cardiovascular disease, with minimal side effects.
- The term “wonder drug” often gets used haphazardly, usually by charlatans to describe unproven supplements. But statins genuinely may be wonder drugs, with few risks but large, life-extending benefits.
There’s been some commotion over the past few years about cholesterol-lowering statins, particularly whether the benefits truly outweigh the risks for the 200 million people who take them worldwide. Much of this discord likely stems from underlying distrust of “Big Pharma” and a misunderstanding of the current state of evidence surrounding statins and cholesterol.
The reason that Lipitor, the first statin and the first truly effective cholesterol-lowering medication, earned Pfizer $150 billion between 1997 and 2017 — making it the top-selling pharmaceutical drug of all-time — is simple: It works. Amazingly well. A doctor once (half?) jokingly remarked, “It’s just a matter of time before they put statins in the water supply.”
Statins: the wonder drug
Most statins like Lipitor are now generic, making their tremendous benefits far easier to affordably access. Statins can lower a patient’s “bad” LDL cholesterol by an astounding 30-50%, translating to a “23% reduction in heart attacks, 17% reduction in fatal or non-fatal stroke, 19% reduction in death from cardiovascular causes, and a 12% reduction in all-cause mortality,” according to a meta-analysis of trials with over 135,000 participants.
Considering that heart disease is the leading cause of death in the U.S., killing 659,000 people each year — that is, 1 in 4 deaths — statins are doing a lot of good. And they accomplish this feat with generally minimal side effects. About one in ten patients will experience muscle aches (which are entirely reversible when use is halted or dosage is decreased), along with a few but rare adverse effects.
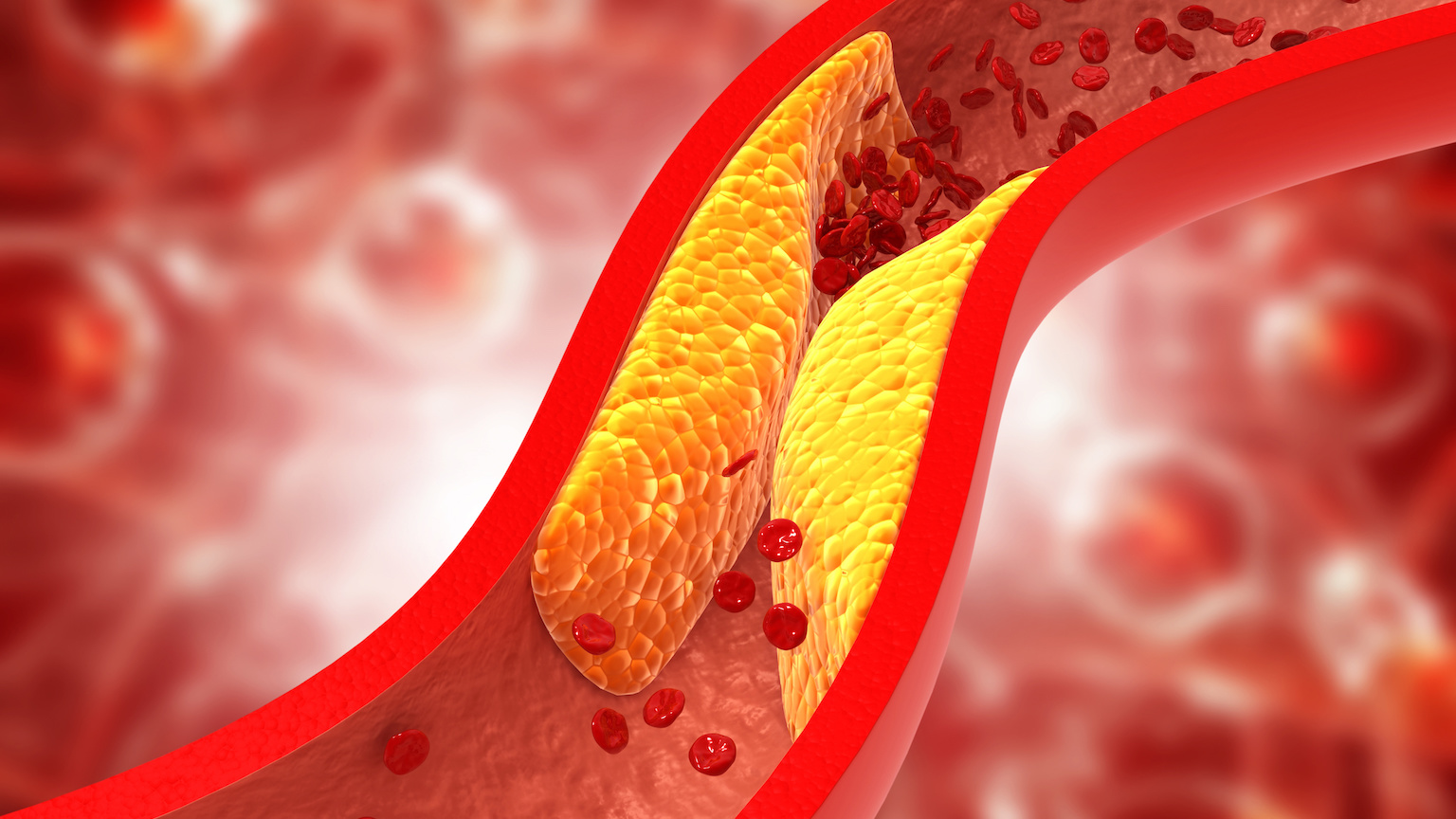
Statins work by reducing low-density lipoprotein (LDL) cholesterol in the body. LDL cholesterol serves a useful purpose, transporting needed lipids (fats) to cells throughout the body, but when there’s too much, LDL can aggregate along the walls of blood vessels, causing them to narrow or even stop flowing entirely. Known as atherosclerosis, this can result in a heart attack or stroke.
And it seems that many of us have too much LDL cholesterol. According to current guidelines, around 60 million Americans are eligible for statins. This includes people who:
“…have clinical atherosclerotic cardiovascular disease, including those with a personal history of stroke, heart attack, or peripheral vascular disease, and also those who suffer from chest pain, have extreme elevations in LDL cholesterol (190 mg/dL or higher), are age 40 to 75 and have diabetes, or are age 40 to 75 and have an estimated 10-year risk of an adverse cardiovascular event greater than 7.5%.” [Emphasis added]
Who should take statins?
It is that final, somewhat confusing category, that draws the most debate, as it could apply to almost anyone over age 65, even relatively healthy people. The gray area leaves room for patients and physicians to have nuanced conversations about statins. Dr. Buzz Hollander, a health writer and family physician in Hawaii, recently offered this reasonable take after wading through the evidence:
“It’s probably better to try first to see if someone can improve their diet, exercise, sleep, stress, and so on. We will never have scientifically sound numbers to put on this, but lifestyle improvements might amount to 50-60% reductions in heart disease risks. They also can carry other benefits, too, like weight loss, fitness, and unearthed joy, which are hard to find in a 40mg atorvastatin pill.”
Dr. Christopher Labos, a cardiologist with McGill University, offered a slightly different, but also reasonable, take at Science-Based Medicine. Noting that it can be very difficult to lower cholesterol with diet and exercise alone, he wrote that “lifestyle changes and medications are not mutually exclusive. You can do both simultaneous [sic] and you probably should.”
While there’s room for these small disagreements, doctors generally agree that statins’ widespread use is entirely called for (though not via the water supply). The term “wonder drug” often gets used haphazardly, usually by charlatans to describe unproven supplements. But statins genuinely may be wonder drugs, with few risks but large, life-extending benefits.