We’re Experiencing a Crisis in Pain Management. Can We Treat It Without Drugs?

I hear about pain all the time. New students introduce themselves with a list of aches and surgeries; old students inform me they’ll be modifying for this or that reason. The factor uniting their issues is pain. They’re either trying to avoid it or strengthen and stretch areas of their body to reduce the pain they feel.
Moving through pain is a relatively recent advancement in America, even though other cultures have advised it for centuries. When I broke my femur in 1986, I spent three months in bed, one in traction, two in a full body cast. Nine months of physical therapy followed. To this day I have an imbalance that in many ways shaped my fitness career: to avoid pain. Today doctors treat femur breaks by having patients walk as quickly as possible. Weight bearing is a more reliable method of healing than weight avoidance, even if a bit of pain is necessary along the way.
So I’m accustomed to members not wanting to rest too long when dealing with an injury. More common is not resting enough, which is a whole other story. But for this story, the general consensus is that we want to feel good throughout our day. We don’t want to lose our breath climbing a set of stairs. We want to pick up our children without our back giving out. We dont’ want our thumbs and neck to hurt after a day on our devices. We don’t want to be in pain.
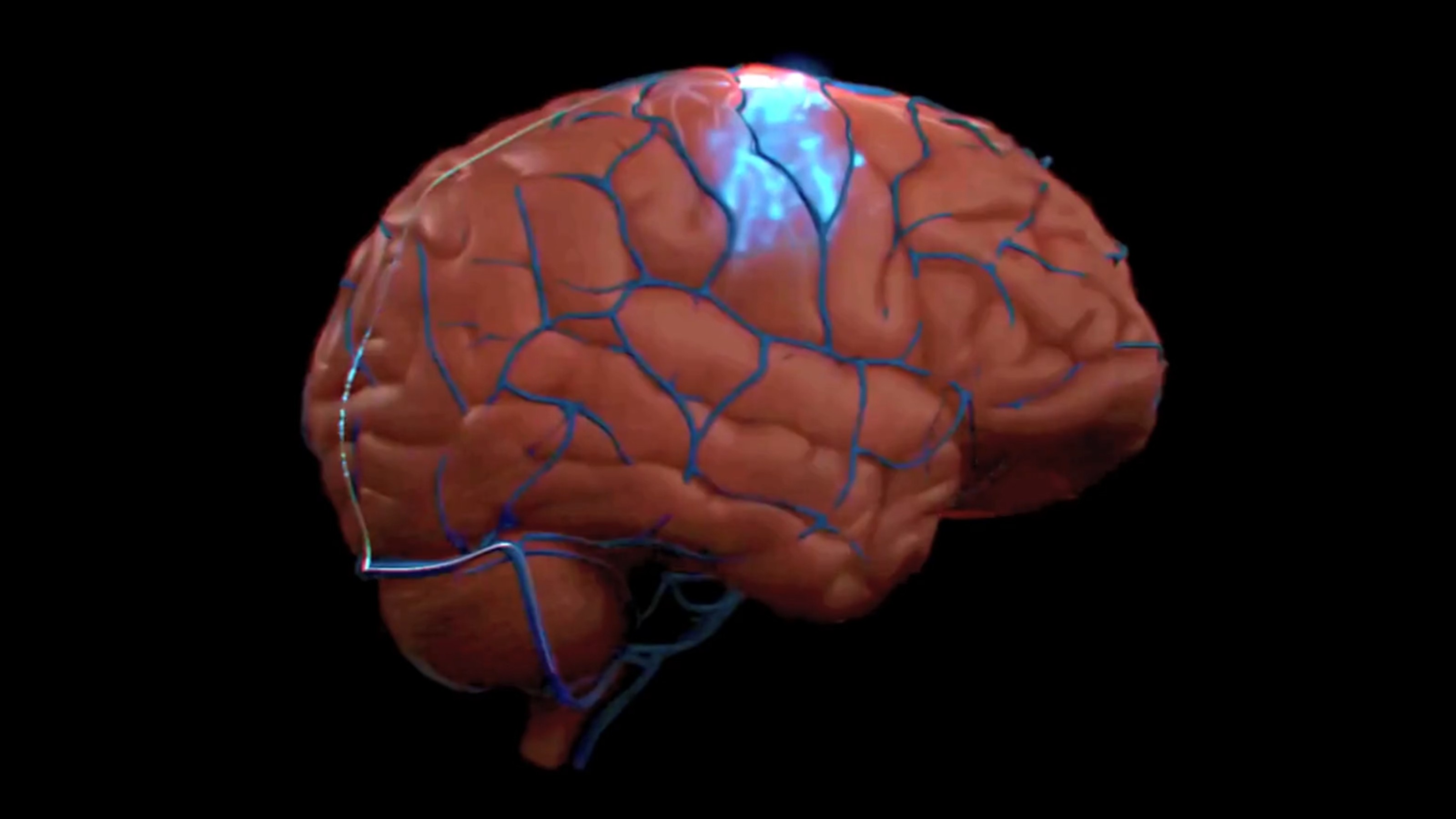
Physical pain is not the only type to harm our bodies. Pain is assessed by our anterior cingulate cortex (ACC), the brain region that gives meaning to troubling bodily signals. Yet the region doesn’t distinguish between stubbing your toe or being rejected by your peers. As neuroendocrinologist Robert Sapolsky writes, “as far as those neurons in the ACC are concerned, social and literal pain are the same.”
Sapolsky implicates neurotransmitter substance p, which relays pain information to the central nervous system, as a “pain-ometer” that communicates signals from not only our skin, muscles, and joints, but also in emotional disorders like clinical depression. Or as he phrases it, “stubbed toe, stubbed psyche.” Our pain networks are so sensitive that even anticipating pain activates our cortical networks.
Unless you can’t feel pain, that is. That’s called CIPA, short for congenital insensitivity to pain with anhidrosis (anhidrosis means you don’t sweat; sweating is a cooling mechanism). This rare genetic disorder disrupts nerve fibers that carry pain, heat, and cold to the brain. This might sound appealing until you realize that bleeding to death from an undetected scrape is a real possibility. CIPA patients are sometimes labelled “fearless,” which means they’re more likely to take physical risks than us pain sufferers, increasing their chances of death.
Pain is an indicator that something is wrong. Yet we’ve learned a lot about how the cortical networks associated with pain work from outliers, such as CIPA sufferers and amputees. Phantom limb syndrome occurs thanks to an error in our brain’s remapping after a limb is removed. Neuroscientist VS Ramachandran famously invented a mirror box that “tricks” amputees into believing they’re looking at their missing limb, which rewires their brain to “relax” networks creating the pain. The box works quite well, where pharmaceutical interventions often failed.
These insights are important because, in many ways, we’re experiencing a cultural crisis in pain management. The opioid crisis is a lesson in pain avoidance. While its roots often are understandable—we don’t want to be in pain—once the brain adapts to the drug, we’re hooked. Trigger warnings and safe rooms are further examples of pain avoidance: this triggers me in an unpleasant way, so I want to avoid it. Avoidance never leads to anything healing.
In response many researchers are actively seeking ways to treat pain without drugs, especially when it comes to one of the most persistent and chronic issues adults suffer from: back pain. The NY Timesreports,
Throwing powerful drugs at chronic pain problems may only add to the problem because ever higher doses are often needed to keep the pain at bay. Knowing this, a growing cadre of specialists are exploring nondrug, noninvasive treatments, some of which have proved highly effective in relieving chronic pain.
Back pain is the number one complaint I hear about at Equinox Fitness, where I teach yoga and fitness classes six days a week. Many members already recognize non-drug treatments—yoga, of course, as well as others now being suggested by the Mayo Clinic: tai chi, progressive relaxation, rehabilitation, mindfulness meditation, and the standard, exercise. Studies in cognitive behavioral therapy and mindfulness meditation are proving to be effective methods for dealing with certain forms of pain.
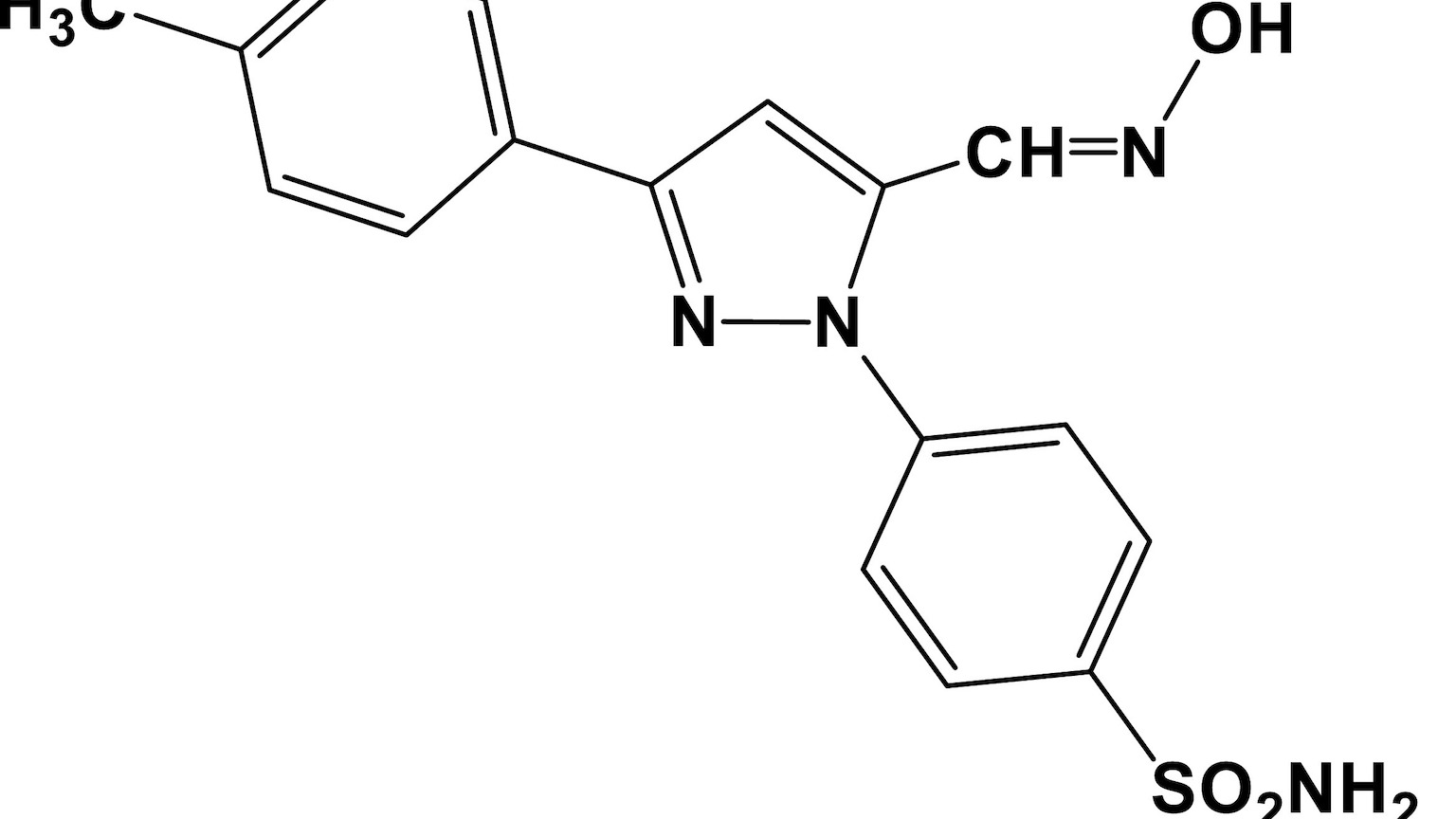
I’ve known many people whose response to the slightest indication of pain is to “pop two Advil.” Ibuprofen is an under-appreciated medical breakthrough, so common has the drug become since its discovery in 1961. Yet temporary relief does not address chronic issues that might need attending to. Soon two become three become four, the doorway to stronger pills just around the corner.
Pain isn’t all in our heads, but inside of our heads resides the organ responsible for how we react to and treat pain. Patience is a necessary response to troubling bodily signals, just as it is for emotional turmoil. This might require trial and error; it might mean suffering a bit of pain until we discover an appropriate method for dealing with it. The cost of pill popping, even seemingly benign over-the-counter remedies, is too high. It rarely addresses the root cause of our pain. Such patience is an important step moving forward, socially, economically, and for our personal well-being.
—
Derek is the author of Whole Motion: Training Your Brain and Body For Optimal Health. Based in Los Angeles he is working on a new book about spiritual consumerism. Stay in touch on Facebook and Twitter.