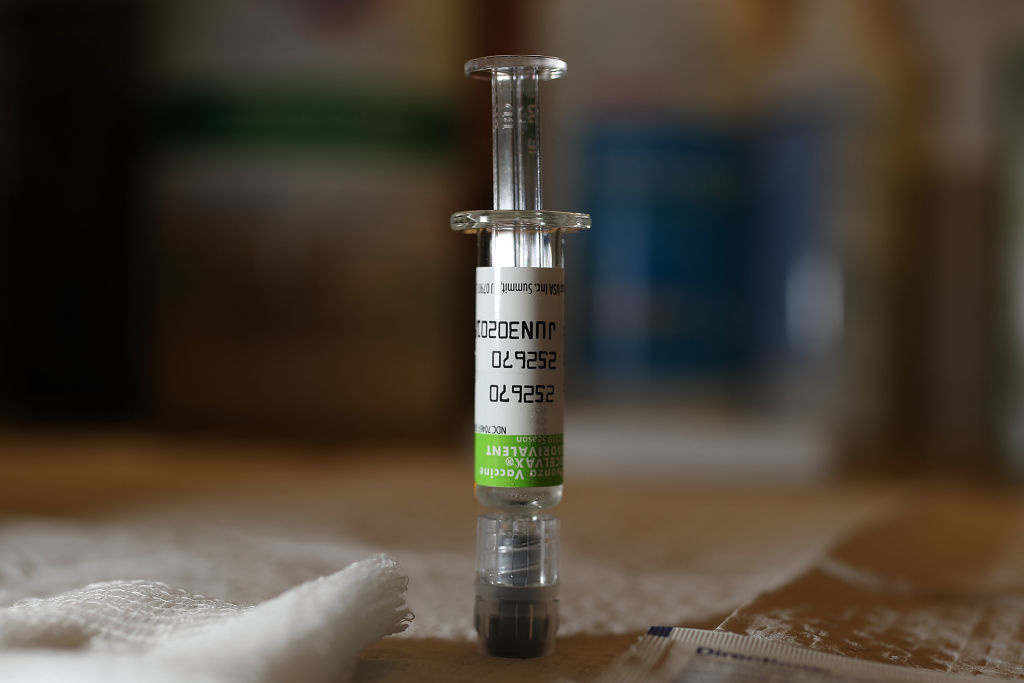
Influenza
A new study at Emory Vaccine Center gets into the bone marrow.
We may never have to get more than one flu shot again.
A measles comeback is not the sort of return our children deserve.
It’s been 100 years since the world’s last deadliest flu pandemic. Experts warn that another one is inevitable, but are we ready?