How psychiatric ideas about trauma evolved after World War I

- Trauma is an emotional reaction to an extremely disturbing event, and it can have lasting effects on the brain and body.
- Although definitions vary, descriptions of trauma-related disorders have emerged from every war since at least World War I.
- Bessel van der Kolk, psychiatrist and author of “The Body Keeps the Score,” spoke to Big Think about trauma and the emerging treatments that are helping people let go of it.
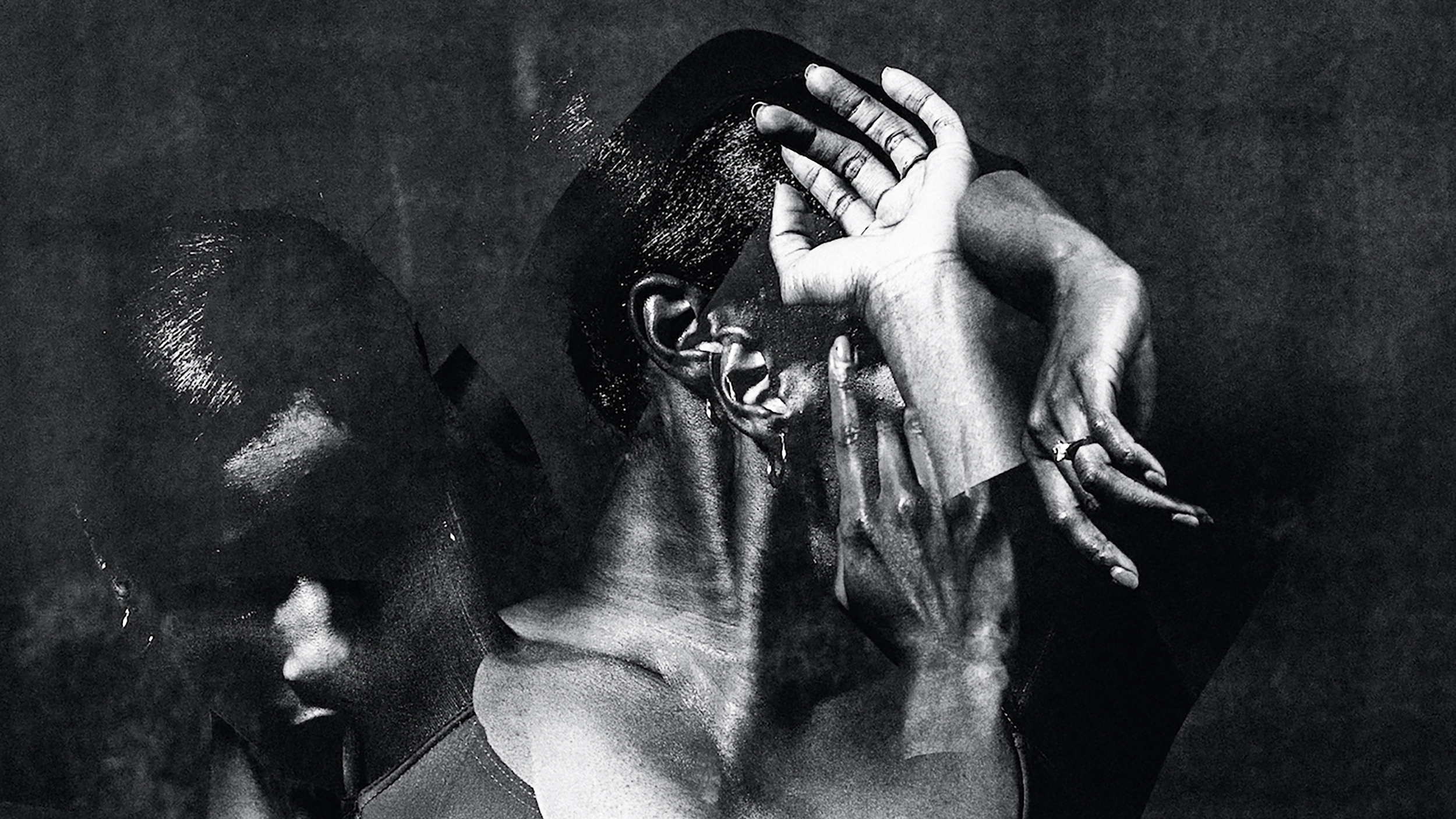
Trauma is a haunting psychological force. Although a traumatic experience may last only a split second, the effects of trauma can echo throughout the mind and body for a lifetime. The lingering symptoms of trauma can manifest in ways that confound both the people suffering from trauma and the medical professionals who treat them.
For the psychiatrist Bessel van der Kolk, the fallout of war brought trauma into clearer focus. In 1978, he began working with veterans of the Vietnam War, which had ended several years prior.
“I was blown away,” he told Big Think. “These were guys who were my age, who were clearly smart and competent and athletic. And they clearly were just a shadow of their former self. But their bodies were clearly affected by trauma and they had a very hard time connecting with new people after the war.”
At the time, however, there was no official diagnosis for trauma-related disorders. That came in 1980 when the American Psychiatric Association first described post-traumatic stress disorder (PTSD) in the Diagnostic and Statistical Manual of Mental Disorders, on which van der Kolk worked as a research assistant.
It marked a controversial turning point in how psychiatrists approached trauma.
“From an historical perspective, the significant change ushered in by the PTSD concept was the stipulation that the etiological agent was outside the individual (i.e., a traumatic event) rather than an inherent individual weakness (i.e., a traumatic neurosis),” wrote Matthew J. Friedman, founding executive director of VA National Center for PTSD.
From “shell shock” to PTSD
Van der Kolk was far from the first psychiatrist to note that extreme violence can warp the psyche. In 1884, the German physician Hermann Oppenheim wrote about the “traumatic neurosis” displayed by people involved in accidents made possible by the Industrial Revolution: train crashes and machine mishaps.
But it took the mechanized horror of the World Wars to bring the idea of trauma into public consciousness. During World War I, psychiatrists were struggling to explain why so many soldiers were unable to function properly even though they had not suffered a serious physical injury. The phenomenon occurred on both sides of the war.
The German psychiatrist Robert Gaupp reported that, following violent artillery battles in 1914, “psychiatric patients make up by far the largest category in our armed forces,” with main symptoms including “states of sudden muteness, deafness […] general tremor, inability to stand or walk, episodes of loss of consciousness, and convulsions.”
The Allied soldiers, suffering from the same constellation of symptoms, coined a term for the condition: “shell shock.” But not everyone believed it existed. Soldiers who displayed symptoms of shell shock or claimed to be suffering from it were often accused of cowardice or malingering. In fact, it is likely that some of the 346 British and Commonwealth soldiers who were executed per military command — due to perceived cowardice or desertion, for example — were actually suffering from PTSD.
But some psychologists supported the shell shock hypothesis. After studying British soldiers with shell shock symptoms in France, the English psychologist Charles S. Myers reported that it was a real condition whose root was psychological and whose symptoms were manifestations of repressed trauma. Myers helped develop the principles of so-called forward psychiatry: the practice of psychologically treating soldiers near the front line with the expectation of sending them back into battle.
The Allied forces used forward psychiatry to treat soldiers in World War II, by which time the term shell shock had been replaced by “combat stress reaction” or “combat fatigue.” These terms differed slightly from shell shock, but the underlying hypothesis was the same: soldiers who suffered from combat fatigue had a weak constitution or a preexisting mental condition.
The Battle of Guadalcanal in 1943 helped to change that. After executing a large-scale offensive, more than 500 Marines returned with symptoms like sensitivity to sharp noises, amnesia, anxiety, muscle tension, shaky hands, and tremors. The American Psychiatric Association called it “Guadalcanal Disorder.” This alarmed military brass: After all, if elite Marines can suffer combat fatigue, everyone is vulnerable.
During the Vietnam War, the U.S. improved its practice of forward psychiatry, suffering far lower rates of psychiatric casualties than in the World Wars. But increased drug and alcohol use might have played a role in temporarily staving off trauma: “The prevalence of delayed and chronic PTSD, in spite of the careful prevention of psychiatric casualties in Vietnam itself, was a rude awakening,” notes a 2000 review of the history of psychotraumatology.
Trauma-related disorders have taken many names over the decades, but the effects have remained essentially the same. Studies of American veterans of the wars in Iraq and Afghanistan suggest that up to 30 percent of soldiers — as many as 500,000 people — have suffered PTSD. The battlefield is unsurprisingly fertile ground for trauma disorders.
But trauma research over recent decades shows that a variety of experiences, physically violent or not, can give rise to trauma-related disorders.
Modern conceptions of trauma
The American Psychological Association currently describes trauma as “an emotional response to a terrible event like an accident, rape, or natural disaster.” It is a broad definition. That is partly because individuals react differently to traumatic experiences; some people have lower thresholds for traumatic experiences, while others might not consider certain experiences to be traumatic. For example, something as seemingly as innocuous as having one’s worldview contradicted can be traumatic for some people.
What is less ambiguous is the prevalence of trauma. A long-term study of trauma among children in the U.S. published in 2018 found that more than 60 percent of children had experienced at least one traumatic event by age 16. The results also supported prior research linking childhood trauma exposure to undesirable outcomes in adulthood: criminal behavior and poor health and social functioning.
“People usually think about the military when they talk about trauma,” van der Kolk told Big Think. “But at least one out of eight kids in America witness physical violence within their parents. A larger number of kids get beaten very hard by their own caregivers. A very large number of people in general, but women in particular, have sexual experiences that were clearly unwanted and that left them confused and enraged.”
How the mind and body store trauma
A sufficiently traumatic experience can cause changes to areas of the brain like the amygdala, hippocampus, and prefrontal cortex. These changes are fueled by an instinct to survive: When you experience a traumatic event, your brain is registering extreme levels of threat, and it does everything in its power to encode the memory so you avoid similar threats in the future.
“Much of the imprint of trauma is the very primitive survival part of your brain that I like to call the cockroach brain, as a part of you that just picks up what’s dangerous and what’s safe,” van der Kolk told Big Think. “And when you’re traumatized, that little part of your brain, which is usually very quiet, continues to just send messages. I’m in danger. I’m not safe.”
This process occurs below the level of rational thought. In many cases, it is beneficial for your brain to automatically respond to threats in the environment. But in excess, trauma can trigger a “recalibration of the brain’s alarm system, an increase in stress hormones, an alteration in the system that filters relevant information from irrelevant,” as van der Kolk wrote in his 2014 bestseller The Body Keeps the Score.
“The problem then becomes that you are not able to engage, or to learn, or to see other people’s point of view, or to coordinate your feelings with your thinking,” van der Kolk told Big Think.
Trauma can cause people to get stuck in flight, fight, or freeze responses, leaving them unable to experience joy and pleasure at healthy levels. And beyond contributing to conditions like anxiety and depression, trauma can also manifest physically: muscle tension, lethargy, fatigue, and even immunological and endocrine abnormalities.
The body, in other words, does not easily forget trauma, even if the mind does its best to suppress the traumatic memory in one way or another. What is the solution? In recent years, van der Kolk has been increasingly interested in treatments that are far less conventional than approaches like antidepressants, whose effects on PTSD he studied in the 1990s and 2000s.
One is yoga, which he said helps encourage you to “pay attention to yourself” and to form a “deep relationship with your internal sensory system.” Another is theater: “It turns out that playing different roles in your body helps you to feel that your body can feel differently, depending on how you organize your relationship to yourself.”
Van der Kolk and a growing number of psychiatrists are also interested in using psychedelics to treat PTSD.
“What we see in the people who get [MDMA] is amazing,” van der Kolk told Big Think. “People are able to go to places they have never felt safe to go. This is not a picnic. They see the horrible things that’s happened to them. But MDMA allows people to see themselves with compassion. All these measures we have about self-perception and self-awareness just shoot up. And rather than blaming themselves, they’re able to say, yes, this what happened to me, but it’s over.”
Still, van der Kolk maintains that no single treatment works alone; it takes a combination of approaches tailored to each individual. The general aim is to process the traumatic experience in a way that helps the brain see the memory from a new — and less threatening — angle.
“Different people need very different things,” he said. “What worked for my last patient very well may not work for you. Everything is an experiment in life. And healing from trauma is an experiment.”