Heart attacks and canker sores: why we need to take oral health seriously

Photo by Carl D. Walsh/Portland Portland Press Herald via Getty Images
- Eighty percent of patients who’ve had heart attacks have gum disease, says Dr. Shahrzad Fattahi.
- Oral health is also implicated in forms of cancer, dementia, canker sores, and more.
- Fattahi says the future of medicine must also focus on saliva, as a whole new field of salivary diagnostics is emerging.
Over the summer, I was sitting in the dentist’s chair, waiting for a cap to be placed over a cracked tooth. While dentist offices rarely inspire joy, I always enjoy visiting Shahzrad Fattahi. Leaving my doctors in New York City was one of the hardest aspects of moving. Thankfully, a mutual friend recommended me to Dr. Fattahi. I gladly travel the extra distance to get to her Playa Vista office—we sometimes forget how much a good doctor matters until we find one.
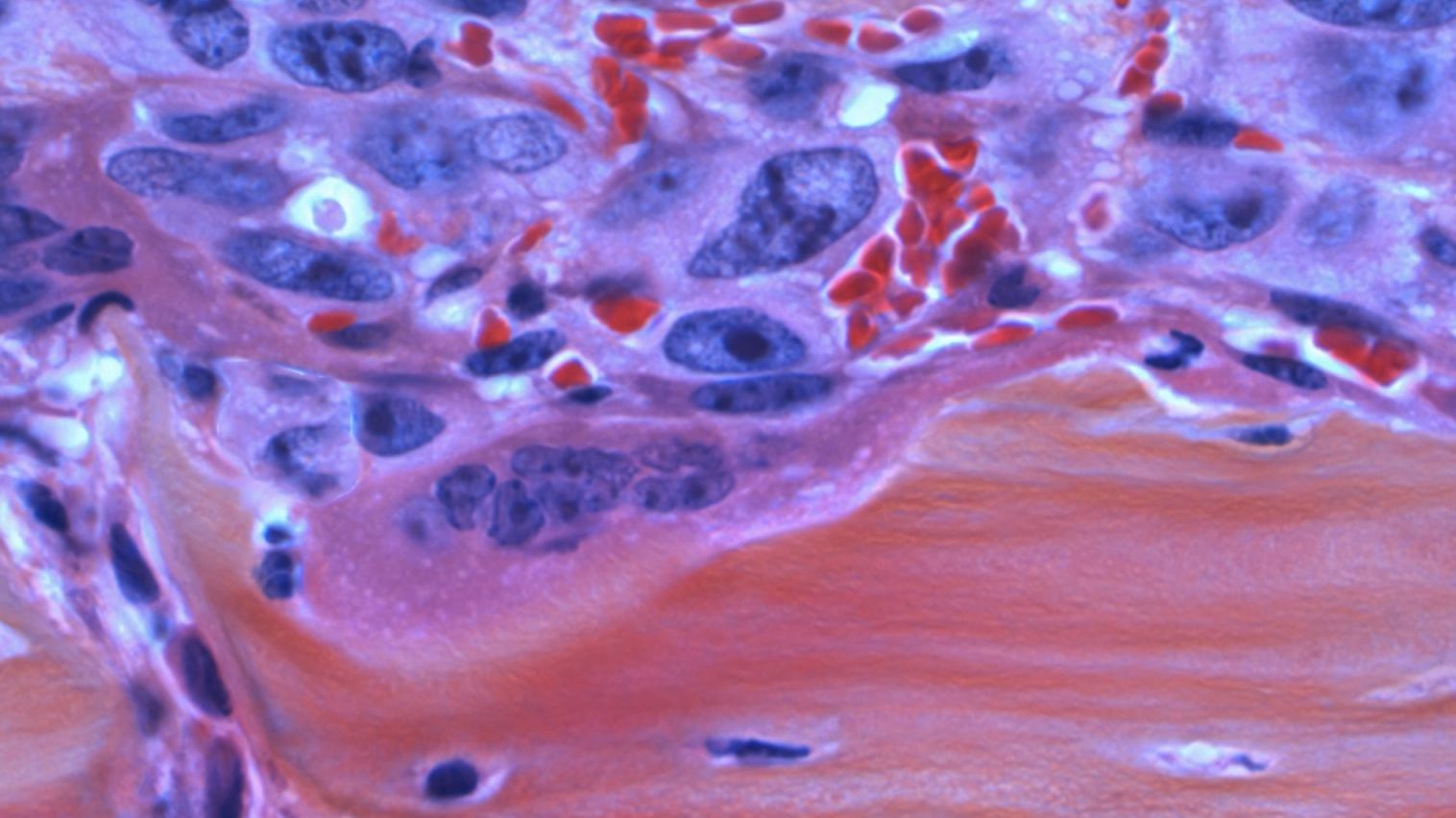
Part of the reason I enjoy our visits is that we end up spending half the time talking about a variety of topics related to health. On this occasion, I mention the microbiome; it’s something I’ve been writing about lately. Dr. Fattahi mentions that the mouth has its own microbiome: Oral health affects a variety of autoimmune disorders, cancers, heart problems, and cognitive issues.
It makes sense. The entryway into our gut microbiome is the mouth. Yet I’d never made the connection about just how important food is from this particular perspective. Gut health begins with salivation. In fact, as you’ll read below, saliva contains nearly as many molecules as blood, making chair-side salivary diagnostics an important part of the future of medicine.
During our wide-ranging discussion (much of which I couldn’t fit into this article), we talk about why dental insurance is separate from medical insurance—one of those givens in America we rarely question—as well as the connection between gut and mouth health, how to promote good bacteria and reduce bad bacteria, why dentistry misses so much by focusing on cosmetics instead of functional health, how oral health affects your breathing, and the best way to help your child develop a strong, healthy jaw for life: breastfeeding.
One thing became clear while I talked to Dr. Fattahi: Holistic health needs to include oral health. Insurance companies need to figure that out, too.

Dr. Shahzrad Fattahi
Derek: In your office, you pointed out the connection between dental health and the microbiome, which is something I had never thought about.
Shahrzad: It’s a great place to start, but maybe we can back up to how dental health affects your whole being and overall health. There is a missing link between what happens in the mouth and what happens in the rest of the body. With our distaste for dental checkups and focus on treatment versus prevention, we really fail to see how dental disease is a warning sign of so many other diseases. We should take a cue from our medical colleagues, who have made a shift toward more functional medicine and looking at root causes of diseases. When you come in for a dental visit now, we are only doing a cleaning, checking for cavities, recommending whitening, and sending you on your way.
We need to move toward functional dentistry. We have so much more information that we can pass on to our patients in terms of their overall health, like salivary testing for your pH levels and your airway assessment. We can do a simple chair-side salivary test to tell you if your bacterial levels are off.
In terms of your microbiome, we all hear so much about gut health, which is really your digestive system. Your gut is now responsible for 80 percent of your immune system and your gut starts in the mouth. If you think of the gut as a long tube, sort of like a conveyor belt, you put the food in your mouth first. Any diet that you follow—keto, paleo, vegan—you’re actually first coating the food with your saliva. If there’s an imbalance, you’re passing that down into the ecosystem along the way. That’s the main way swallowing bacteria is going to further affect your immune system downstream.
Derek: And you start salivating before you even begin eating. Sometimes a trigger, such as thinking about food, can make you salivate.
Shahrzad: Absolutely. The first part of your digestive system is the salivary enzymes that are exuded from your salivary glands. You activate your vagus nerve the first time you swallow, which activates the rest of your digestion. What’s important to understand is that we’re not saying “antibacterial.” We are saying you should have a balance of bacteria. Imbalance causes the dysbiosis between the good and bad bacteria.
Interview with Dr. David Wong on Salivary Diagnostics
Derek: What causes bad bacteria in your mouth?
Shahrzad: Good and bad bacteria is divided into two groups: the slow eaters and the fast eaters. The fast eaters feed on simple carbohydrates like sugars. When we eat sugary, white flour foods, we send these back bacteria into a frenzy. Then they metabolize acids. The slow eaters are actually the ones that are designed to digest longer, more complex molecules. They feed more on fibrous fruits.
Derek: Good and bad in this sense are based on the foods you’re eating. When you say slow, it’s not necessarily the amount of times you chew, but the actual foods you’re consuming?
Shahzrad: In part, yes, definitely the foods that you’re consuming. Processed foods, white sugars, and grains tend to see the faster-metabolizing bacteria. The more fibrous foods tend to affect the more slow-growing bacteria. If you eat too much sugar, the fast-metabolizing strains multiply too rapidly and spew out too much acid. That starts a chain reaction that leaches too much calcium from the enamel. The fastest-growing bacteria grow at the expense of the slower-growing bacteria.
If you have an imbalance, for example, if you have a lot of stress, we know that cortisol tends to secrete from the fluid around your teeth. That leads to the growth of gingivalis, which is the main bug that causes all the problems that we are seeing with GI.
Derek: What is it psychologically that people don’t like to or are afraid to go to the dentist?
Shahzrad: We have to talk about the fear and trauma around dentistry. I was a kid in the seventies. We didn’t grow up in a very kind, nurturing environment. Usually they would kick your mother out, tell you to be quiet and just suck it up, and you would be sitting helpless on the chair. More than anything, I hear every day, “Doc, I don’t want to be here. I’m so afraid.” The dentist appointment is the last phone call anyone makes. You’re not thinking of your dental appointment as part of your health.
Most of the calls I get are pain calls. You tend to only go when you’re in pain. Organized dentistry is now making a more concerted effort to create nurturing environments.

A dentist treating a soldier, Trench Mortars School, Nervesa della Battaglia, World War I, Italy, 20th century.
Derek: How do we get people to understand that oral health affects overall health?
Shahzrad: We have so many studies linking all kinds of periodontal disease and gum disease. There are links between gum disease and heart disease. In fact, 80 percent—this is a staggering number—80 percent of patients who’ve had heart attacks have gum disease, yet there’s no discussion between dentists and cardiologists. We now have evidence of Alzheimer’s being linked to gum disease. We now show increments of the same bacterial colonies in the intestine of patients with HIV, colon cancer, GI, and pancreatic cancer. The science is there.
Derek: We’re really just learning how important gut health is. You’re adding another layer here. The “tongue microbiota” is a new term to me.
Shahzrad: Yes. And we need to have more of these discussions. We need to make a paradigm shift to thinking about oral health as valuable and a part of our overall health. As our food got softer and less nutrient-dense, not only did we stop eating less roughage, we stopped using the muscles of our faces. We also started to eat a more grain-based diet, which is lacking in fat-soluble vitamins like A, D, and K. We also see in our patients a higher incidence of canker sores. If you’re low in Omega 3s, you may be having periodontitis.
Derek: Cooking, however, made foods more nutritionally bioavailable. Richard Wrangham wrote an excellent book on that topic. The trade-off, of course, was that our jaws got much weaker.
Shahzrad: It’s like going to the gym and exercising your muscles. The more you exercise, the better muscle strength and overall bone bone density improves. It’s the same with the jaw. You want to eat more fibrous foods, but also foods that are nutrient-dense, that have K2 and vitamin D.
Derek: I used to have regular outbreaks of four to six canker sores at a time. When I went from a longtime, grain-heavy vegetarian diet to eating meat again, my canker sores disappeared. I haven’t had one in four years now; I know there is a link there. This is just one example of the importance of food and your mouth. Overall, what is the future of oral health?
Shahzrad: The field of salivary diagnostics has come so far. Saliva markers can be used to detect all kinds of diseases, oral cancer, breast cancer, all kinds of autoimmune diseases. Chair-side salivary testing, which we offer in our practice now, will be the new paradigm, not only in the dental field but in the whole medical field. Dr. David Wong at UCLA is doing some very exciting research. He published 165 million genetic sequences and found that saliva contains many of the same molecules contained in blood. In the future, if you’re not looking at saliva, you’re going to be missing indicators of disease.
—
Stay in touch with Derek on Twitter and Facebook.