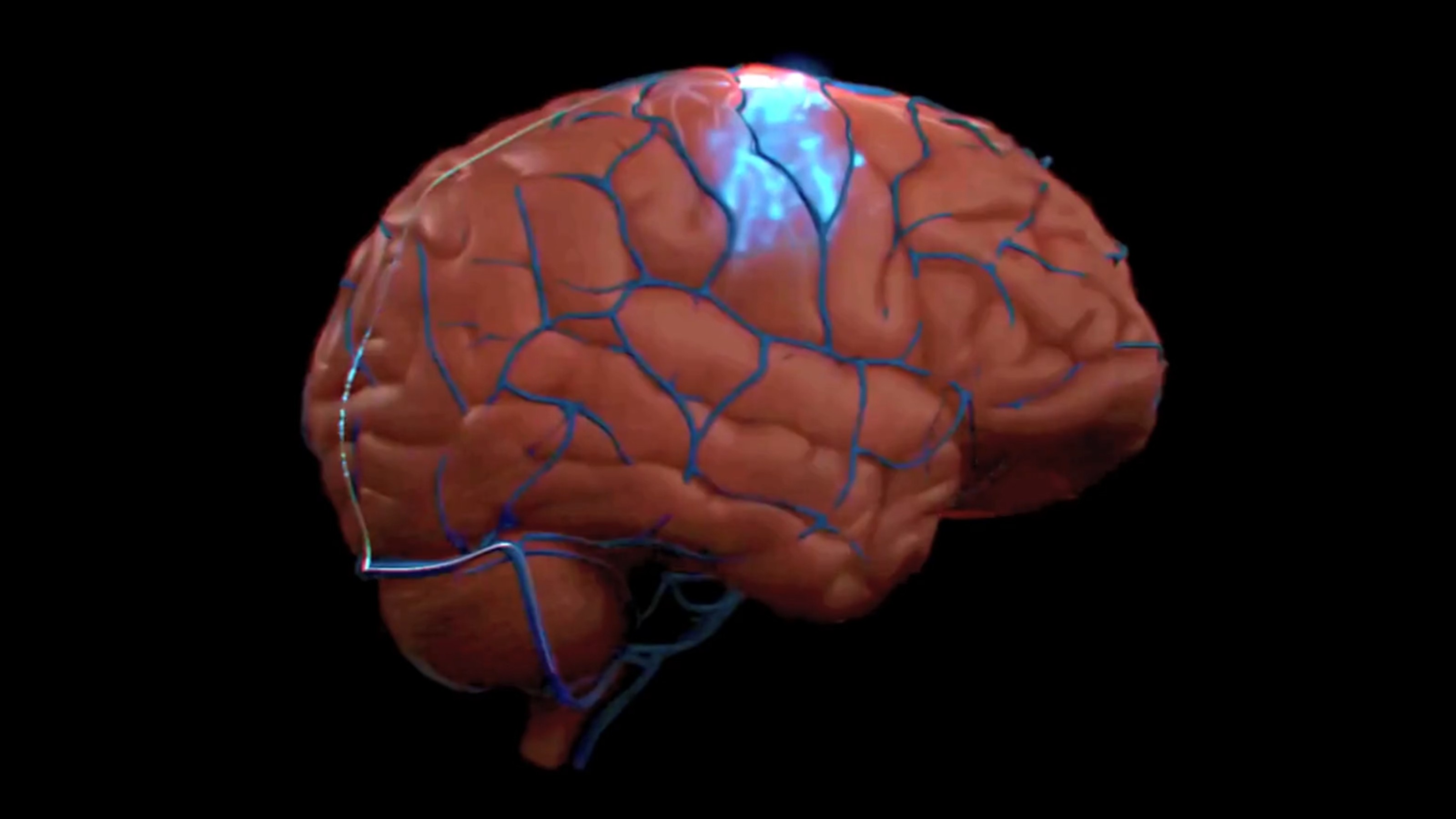
Lung Cancer: To Screen or Not to Screen?

We baby boomers may be getting a little long in the tooth, but we sure know how to take good care of ourselves. Or do we?
One of the greatest health threats we face is one over which we have limited control: lung cancer, the greatest cancer killer even among non-smokers. It was once thought that X-ray screening provided prophylaxis, but later studies showed absolutely no benefit, and possibly even harm for this modality. On Nov. 4, 2010, a large NIH trial reported that the much more sensitive CT imaging yielded a striking 20% reduction in mortality for the sampled group comprising smokers over 55 years of age. Evidently, CT scans can detect tumors early enough for their successful surgical removal. To be fully reliable, the data will have to be replicated, and the first repeat has already been reported at the University of Cincinnati. It is reasonable to suppose that screening would work just as well in non-smokers. So assuming that the results are correct and generally applicable, how can we decide what is an actionable course to pursue right now?
It may be useful to compare this example to the biggest success story in cancer screening to date—colonoscopy for colon cancer. Anyone over 50 years of age who does not have this procedure done roughly every five years is taking an unnecessary health risk. The work-up and screening involved in a colonoscopy is much more invasive and time consuming than a CT scan. Then why isn’t this an open and shut case in favor of the CT lung screen? The answer relates to what happens next in cases of a positive test result. For colonoscopy, any growth is removed during the procedure, period. But for CT screening, positive testing would require follow-up of biopsies and, if necessary, surgery. Whether this follow-up poses an unwieldy burden for the individual and for society (not identical calculations) will depend critically on the rate of false positives. A high false positive rate would impose a huge cost, including exposure to any danger imposed by the screen itself.
But shouldn’t the medical community be striving to stack the odds in favor of screening by making improvements? For example, they could refine the screening and interpretation of test results to yield the lowest possible rate of false positives. And also they could streamline and simplify follow-up procedures, such as biopsies (perhaps these could be done by a needle during the CT scan itself). Some progress along these lines has already been reported in the Cincinnati study.
Still, the question remains: what is actionable right now? Like many medical decisions, we must operate in a world of incomplete information and uncertainty. My own plan is to ask my doctor at the annual physical whether I can have the CT screen done, after researching locations and reputations of screening centers. This would likely not be covered by insurance, but the screen should not cost more than several hundred dollars. Absent an overall lung cancer strategy within the medical community (see preceding paragraph), a course of action following the dreaded positive result would be decided upon if and when it occurs. Among the many medical decisions we make, preventive steps can be the most confounding. But it is critical to be aware of available information and start to crunch our internal numbers to arrive at a plan that is wise and timely to meet our individual needs.
Image courtesy of Flickr user socialisbetter.