Ketamine infusion: The new therapy for depression, explained

Credit: COLE BURSTON via Getty Images
- Ketamine is the first hallucinogen approved for therapeutic use in the U.S.
- Research has shown ketamine is effective at treating depression.
- Though ketamine infusion therapy is now being offered at hundreds of North American clinics, there are unaddressed dangers in the current ketamine gold rush.
In March 2019, the FDA approved ketamine, under the trade name Spravato (esketamine), for clinical use in treatment-resistant depression therapy. Alongside racemic ketamine, which is commonly used in ketamine infusion therapy, ketamine is the first hallucinogen approved for therapeutic usage in the United States.
Technically, ketamine is not a psychedelic but rather a hallucinogen and dissociative. (While ketamine has psychedelic effects, traditional psychedelics bind to the 5-HT2B receptor.) Still, advocates for psychedelic therapy recognize ketamine as a gateway for traditional psychedelics, such as psilocybin and LSD, to be considered for therapeutic usage.
To understand the proliferation of ketamine clinics across North America, the origins of this peculiar substance — one that went from battlefields to veterinary clinics to dance clubs in the span of two decades — must be discussed.
History of ketamine
In 1962, chemistry professor Calvin Stevens synthesized ketamine while researching alpha-hydroxyimine rearrangements. The first human tests were conducted on prisoners in 1964. Ketamine soon replaced phencyclidine (PCP) as the go-to anesthetic in hospitals. It was initially used on soldiers during the Vietnam War following FDA approval in 1970. Thanks to its success on the battlefield, ketamine was placed on the World Health Organization’s List of Essential Medicines.
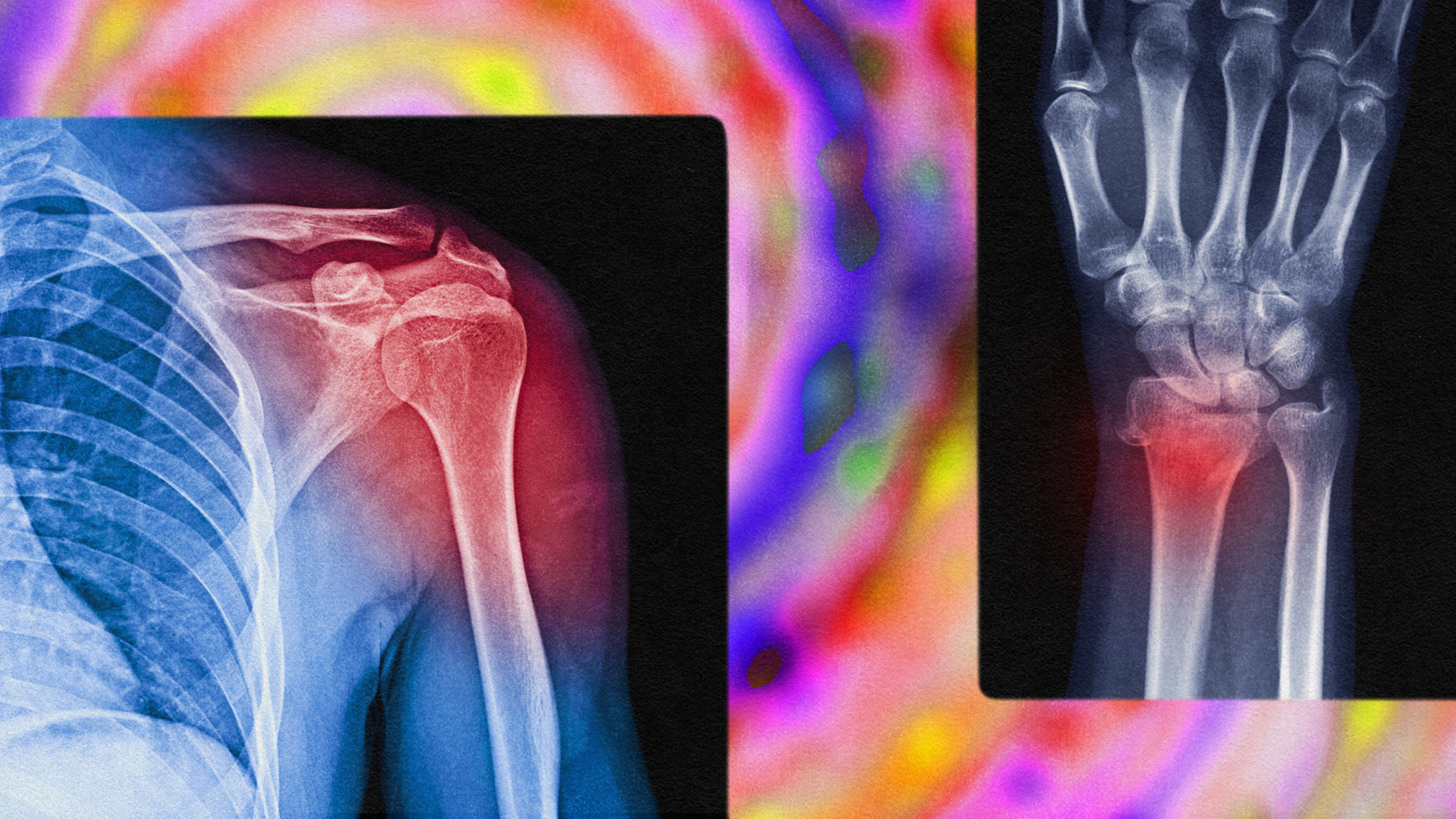
Ketamine has been used broadly as a sedative and anesthetic; to aid in emergency surgeries in war zones; as a bronchodilator for severe asthmatics; to treat certain types of seizures; and in postoperative pain management. Now, ketamine infusions and nasal sprays are being used for depression. Ketamine is also showing potential efficacy in treating chronic pain and suicidal ideation, though more research needs to be done.
Of all of those uses, ketamine has predominantly been used as an anesthetic in humans and animals. While it restricts breathing less than other similar medications, ketamine also produces hallucinations (thus, it’s labeled as a dissociative anesthetic). The list of potential side effects from using ketamine is long, including nausea, double vision, breathing problems, impaired memory, liver enzyme abnormalities, urinary tract problems, and even increased depression — an alarming possibility given its growing use as an antidepressant replacement.
Small-scale studies on using ketamine to treat depression were conducted in 2000 and 2006. Further research confirmed its role in alleviating depressive symptoms, including the possibility that the antidepressant effects of a single dose can persist for weeks. In 2016, the FDA fast-tracked ketamine trials for depression.

Ketamine infusion therapy
There has yet to be a consensus on how ketamine addresses depression. Antidepressants act on the body’s serotonin and noradrenaline systems. Ketamine seems to interfere with an amino acid derivative, NMDA. As a 2017 study published in the journal Nature explains:
“Ketamine is responsible for blocking the N-methyl-D-aspartate (NMDA) receptor, which causes an immediate alleviation of depressive effects, while another metabolite in the drug helps the effects last for hours. This blockage is also what causes the hallucinogenic effects.”
Small intravenous doses of esketamine — an enantiomer of ketamine and the substance actually approved by the FDA — seem to lift depressed patients out of their funk. So does Spravato, a nasal spray that can only be administered under supervision in a doctor’s office or clinic.
Patients that have tried two different antidepressant medications with no success (the definition of treatment-resistant depression) can legally receive ketamine infusions or Spravato at clinics located all over the country. Since the therapy is generally not covered by insurance, treatments range from $300 to $2,000 per session; the Field Trip Treatment Program, which includes psychotherapy and six infusions, runs $4,700.
The process of ketamine infusion therapy is varied depending on which clinic you attend. Companies like Field Trip and organizations such as MAPS require psychotherapy sessions to coincide with infusions.
Unfortunately, therapeutic implementation has not always lived up to federal requirements. Reports of patients quitting antidepressants and psychotherapy to use esketamine as their primary source of treatment abound. Since medical professionals with no mental health training, such as nurse practitioners, anesthesiologists, and pain physicians, can legally administer ketamine, patients are left to process the drug’s effects with little to no guidance.
Thus far, efficacy has been mixed. As STAT News editor Megan Thielking writes, people with minor depressive issues are likely better candidates for ketamine therapy than those with treatment-resistant depression, the very cohort the drug is purported to target.
“Studies vary but have found response rates to ketamine as high as 70 percent among people with major depression who have failed a few other antidepressants. But the rate is lower for patients with extremely treatment-resistant depression, and how long any improvement lasts varies from one patient to the next.”
Was ketamine approved too quickly?
While ketamine therapy is certainly promising, the FDA-approved trials raise a number of red flags. A recent analysis in The British Journal of Psychiatry concludes that we’re moving too fast. Author Mark Horowitz writes:
“Out of the three short-term trials conducted by Janssen only one showed a statistically significant difference between esketamine and placebo. These were even shorter than the 6-8 week trials the FDA usually requires for drug licensing.”
Trials usually last three months; the approved ketamine trials only lasted four weeks and barely showed efficacy above placebo. More concerning, the FDA allowed Janssen to submit a discontinuation trial with a study design flaw as evidence of efficacy — side effects were treated as evidence of relapse, not withdrawal symptoms. Even more alarmingly, six people in the esketamine group died during the trials, including three by suicide, two of which had previously shown no signs of suicidal ideation.
When Janssen stated that the problem wasn’t esketamine but underlying conditions, the FDA accepted the reasoning even though no conclusive evidence was provided. This doesn’t mean ketamine therapy isn’t potentially therapeutic, though it does suggest that its approval by the FDA was rushed.
Psychiatrist Lori Calabrese, who offers ketamine infusion for depression and anxiety in her clinic, puts it best when stating, “The pace of ketamine treatment in real-world practices has outstripped what researchers are able to do and publish.” Time will tell if this treatment proves more beneficial than dangerous in mental health treatments.
—
Stay in touch with Derek on Twitter and Facebook. His most recent book is “Hero’s Dose: The Case For Psychedelics in Ritual and Therapy.”