Malaria resistance shows that mutations are not always random
- Natural selection relies on randomly generated, beneficial mutations that confer a fitness advantage on an organism.
- A specific hemoglobin mutation, called HbS, can make humans resistant to malaria.
- The rate of HbS mutation appears to be non-random and is higher in regions where malaria is more common.
Charles Darwin ruined the chicken and egg paradox. When the Greek philosopher Plutarch posed the question, “Which came first: the chicken or the egg?” he was describing a situation in which cause and effect are unclear. Although Plutarch’s question is metaphorical, evolutionary biology provides a literal answer: the egg.
This answer is supported by the Darwinian principle that offspring are born with new traits that the parents did not possess. Essentially, the first animal to lay a chicken egg was a proto-chicken — a bird similar to a modern chicken, but not quite a chicken. When the proto-chicken created genetic material for the egg, a few random mistakes (mutations) occurred. As a result, the organism inside that egg had mutations that the proto-chicken did not have. Because of these de novo mutations (that is, new mutations that appear in offspring but not in the parents), a chicken would emerge, not a proto-chicken.
For the past century, scientists have assumed that de novo mutations occur randomly and that natural selection favors beneficial mutations. Over millennia, the accumulation of these individual, beneficial mutations allows complex structures to gradually evolve from simpler structures. This assumption of gradual accumulation sits at the heart of evolutionary theory.
A team of researchers from Israel and Ghana has challenged this assumption. In a recently published study, they presented the first evidence that some de novo mutations do not occur randomly.
Malaria: An ancient force of human evolution
In just the 20th century, malaria killed 150 to 300 million people. It should not be surprising, therefore, that malaria is one of the oldest and strongest forces of natural selection that humans have faced.
As a result, humans have evolved various traits that make them more resistant to malaria. Unfortunately, most of those traits come with a cost. For example, individuals are 50% to 90% more resistant to malaria if they possess a specific mutation in their hemoglobin gene. However, if the individual has two mutated versions of the gene, they develop sickle-cell anemia — a condition in which blood cells cannot carry oxygen effectively.
Scientists have long assumed that the “hemoglobin sickle-cell” (HbS) mutation arose randomly in an individual in sub-Saharan Africa. Because of its malaria-protective benefits, that individual’s offspring would have been more likely to survive and reproduce. Thus, the HbS mutation spread inside Africa where malaria is common.
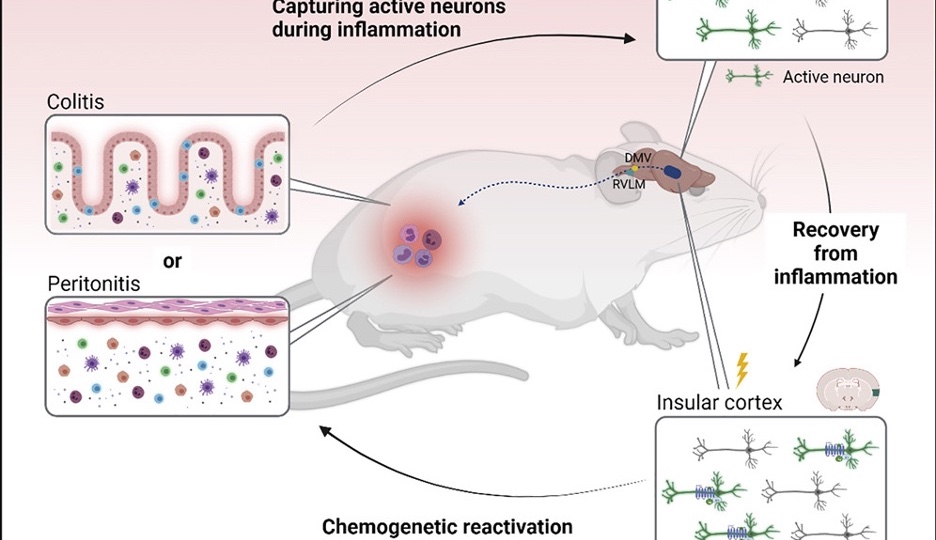
However, Adi Livnat, the expert in evolutionary biology who led the groundbreaking study, suspected that the origin of HbS is a little more complicated than a single random mutation. Instead, he hypothesized that humans have evolved a complex mechanism (through many random mutations), the purpose of which is to generate more mutations. Though these driven mutations would also be at least somewhat random, they would also be intentional.
Why does it need to be this complicated? Because useful mutations aren’t useful all the time.
Malaria is spread by mosquitoes, and mosquitoes flourish during warm periods. The last Ice Age ended about 10,000 years ago, and mosquitoes were thrilled. Some centuries were especially warm. During those periods, there were more mosquitoes and, consequently, more malaria. Hence, a mutation that guarded against malaria would be very beneficial.
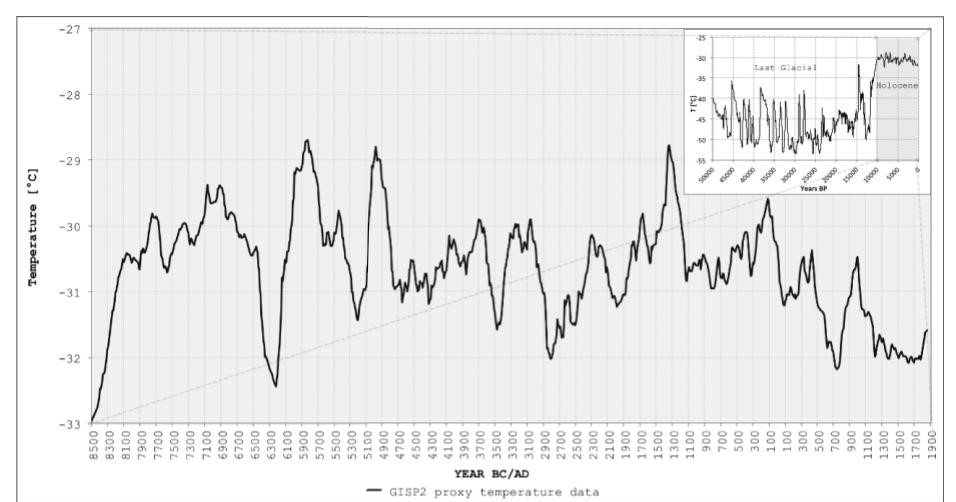
However, during the cold periods when there were fewer mosquitoes and less malaria, HbS provided no benefit. More importantly, sickle-cell anemia was dangerous and not worth the risk. Now, having the mutation was potentially detrimental. If the HbS mutation arose randomly in an individual in sub-Saharan Africa, then the likeliest outcome is that it would vanish during cold periods.
But that’s no good. We know that the climate will warm up again and malaria will return. If a mutation-generating mechanism evolved, as Livant hypothesized, then that mechanism could cause the HbS mutation in response to environmental changes. Essentially, this would allow the mutation to be lost when it provided no benefit and quickly and intentionally regained when it did provide a benefit.
Testing the hypothesis
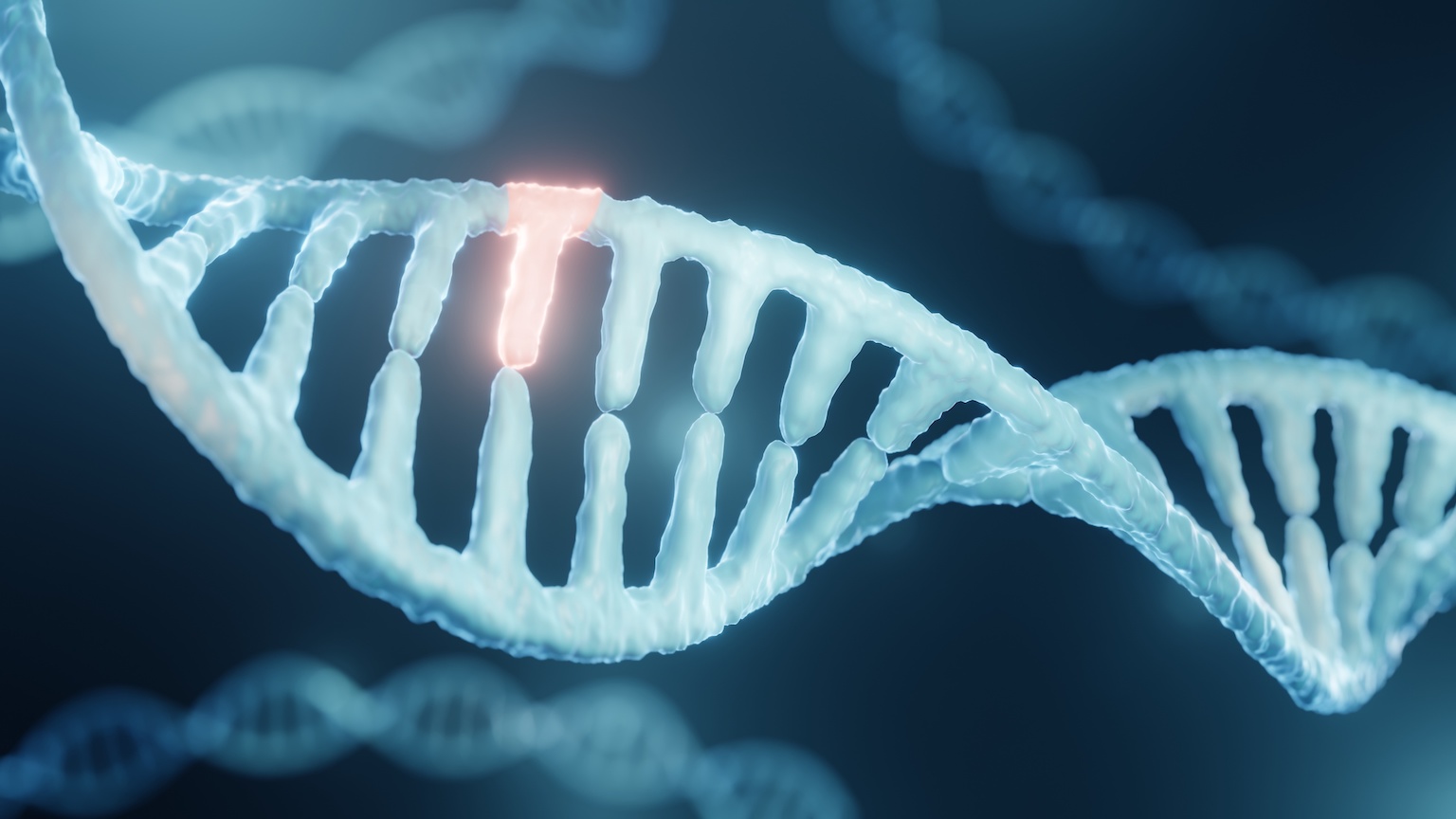
In theory, Livnat’s hypothesis is easy to test. First, analyze DNA from people without the HbS mutation from two different environments: a region where malaria is common (such as central Africa) and a region where it is uncommon (such as north Europe). Then analyze the DNA of their children.
If HbS arises randomly, then the HbS mutation will be equally common in the children, regardless of their parents’ environment. If, however, Livnat’s hypothesis is correct and HbS mutation is non-random, then the children of parents who lived in central Africa will be more likely to have a de novo HbS mutation.
In reality, this is not easy to test. De novo mutations in humans are extremely rare. Usually, a child’s genome contains around 74 de novo mutations. To put that in perspective, if a person possessed a mechanism that made them 1,000x more likely to have a de novo mutation (which is astronomically high), then that person would need to have 40,000 children for one child to have the HbS mutation.
One human does not produce that many children, but males produce tens of millions of sperm cells each day. So, Livat and his team acquired 11 sperm samples: seven from African donors and four from European donors. Each donor provided around 30 million sperm cells, and none of the donors had the HbS mutation.
Yet, the HbS mutation appeared nine times in sperm from African donors but not at all in the sperm from European donors. The team calculated the de novo mutation of HbS to be 35 times greater than average in the sperm of these African men. Importantly, the researchers confirmed that the African donors were not naturally prone to de novo mutations in general. To do this, they determined the rates of de novo mutation in a control gene and found no difference between the two donor groups.
For both populations, the hemoglobin gene (and adjacent genetic sequences) are identical, yet the mutation rates vary significantly between the populations. Thus, the researchers concluded that something other than this local DNA sequence affects these mutation rates.
“The results suggest that complex information that is accumulated in the genome through the generations impacts mutation, and therefore mutation-specific origination rates can respond in the long-term to specific environmental pressures,” said Livnat. “Mutations may be generated nonrandomly in evolution after all, but not in the way previously conceived.”
Livnat’s finding will have to be tested further, but it has the potential to revolutionize our fundamental understanding of evolution.