Battling “butterfly disease”: Experimental therapy successfully regenerates skin

- The skin of individuals with butterfly disease blisters at the slightest touch, due to a lack of a skin protein.
- Doctors employed a risky and experimental procedure to replace nearly all of a patient’s skin with stem cells genetically modified to produce the lost proteins.
- Five years later, the patient seems to be functionally cured of butterfly disease and exhibits no side effects.
In June 2015, a 7-year-old child named Pat was admitted to the Burn Unit of the Children’s Hospital in Bochum, Germany with blisters and open wounds covering almost 60% of his body. Pat was not the victim of a fire, but rather a rare disease called epidermolysis bullosa, commonly known as butterfly disease. The slightest friction — rubbing against bed sheets or bumping into a door — could cause Pat’s skin to erupt in blisters or even slough off, leaving open wounds. These lesions weren’t a new experience for Pat; they’d besieged him for all of his short life. But they had never been this bad, and it was only getting worse.
Weeks turned into months as Pat’s doctors tried to improve his condition, but they were fighting a losing battle. Every therapeutic strategy failed. The wounds spread to cover 80% of his body. There was only one remaining option: an experimental technique that had only been attempted twice, but never under such critical conditions.
For the past five years, Pat has returned to his doctors — not to seek treatment, but because, against all odds, he appears to be the first person to ever be cured of butterfly disease.
Preface: The butterfly disease
Pulling off a Band Aid can feel like you’re ripping skin off. For those who suffer from Butterfly Disease, that’s exactly what happens. In healthy skin, anchor proteins tightly link the outermost layer of skin (the epidermis) to an underlying layer (the dermis). Ripping off a Band Aid won’t cause these layers to separate. However, repetitive rubbing — for instance, due to a poorly fitted shoe — will eventually break apart the anchor proteins, and blisters will form as fluid fills the space between the two now-separated layers.
People born with butterfly disease don’t produce the vital anchoring proteins due to a rare genetic mutation. Since there is no protein to hold the two skin layers together, minor mechanical trauma (like pulling off a Band Aid) can peel apart the layers of the skin, resulting in blisters and painful open wounds.
Roughly 100 babies are born with this condition each year, and nearly half die before they reach adolescence. Treatment options are limited: prevent infections of open wounds, manage the pain, and wait for the body to heal itself. But sometimes, as in Pat’s case, that just isn’t enough.
Act one: The losing battle
When Pat arrived at the hospital, blisters and sores covered over half his small body. But this wasn’t what brought him to the hospital; for Pat, lesions were the norm. A fever, on the other hand, was a grave concern. It indicated that Pat was battling an infectious disease as well. It seemed that the butterfly disease had acquired bacterial allies.

Seven years of battling Butterfly Disease had taken a toll on Pat’s body. He weighed a mere 37 lbs (the average weight for a 7-year-old is 50lbs). The body devours nutrients when healing wounds, and with the arrival of two of the most notorious pathogens, Staphylococcus aureus and Pseudomonas aeruginosa, the nutrient demand would only increase. In other words, Pat’s body was under siege from multiple fronts, and his body’s capacity to protect itself was already dangerously strained. Luckily, Pat had allies.
For weeks, a team of doctors and nurses helped Pat fight against the microbial invaders. But each therapeutic tactic was met with complications. They had to bathe Pat in disinfectant every other day; the pain of which was so excruciating that he had to be under general anesthesia — a significant risk, given his critical condition. New wound dressings were applied daily. However, as the dirty dressing were removed, the exposed lesions bled and leaked fluids, so Pat required weekly blood transfusions. They monitored for new infections and customized antibiotic treatments strategies accordingly. But with open wounds covering 60% of his body (and expanding every day), it was proving impossible to prevent new infections and turn the tides of the battle.
Pat’s condition continued to deteriorate, as did his chance of recovery. They needed a new tactic. His doctors proposed an experimental procedure. And while a child’s life should never be an experiment, it was the only remaining option.
Act two: The only remaining option
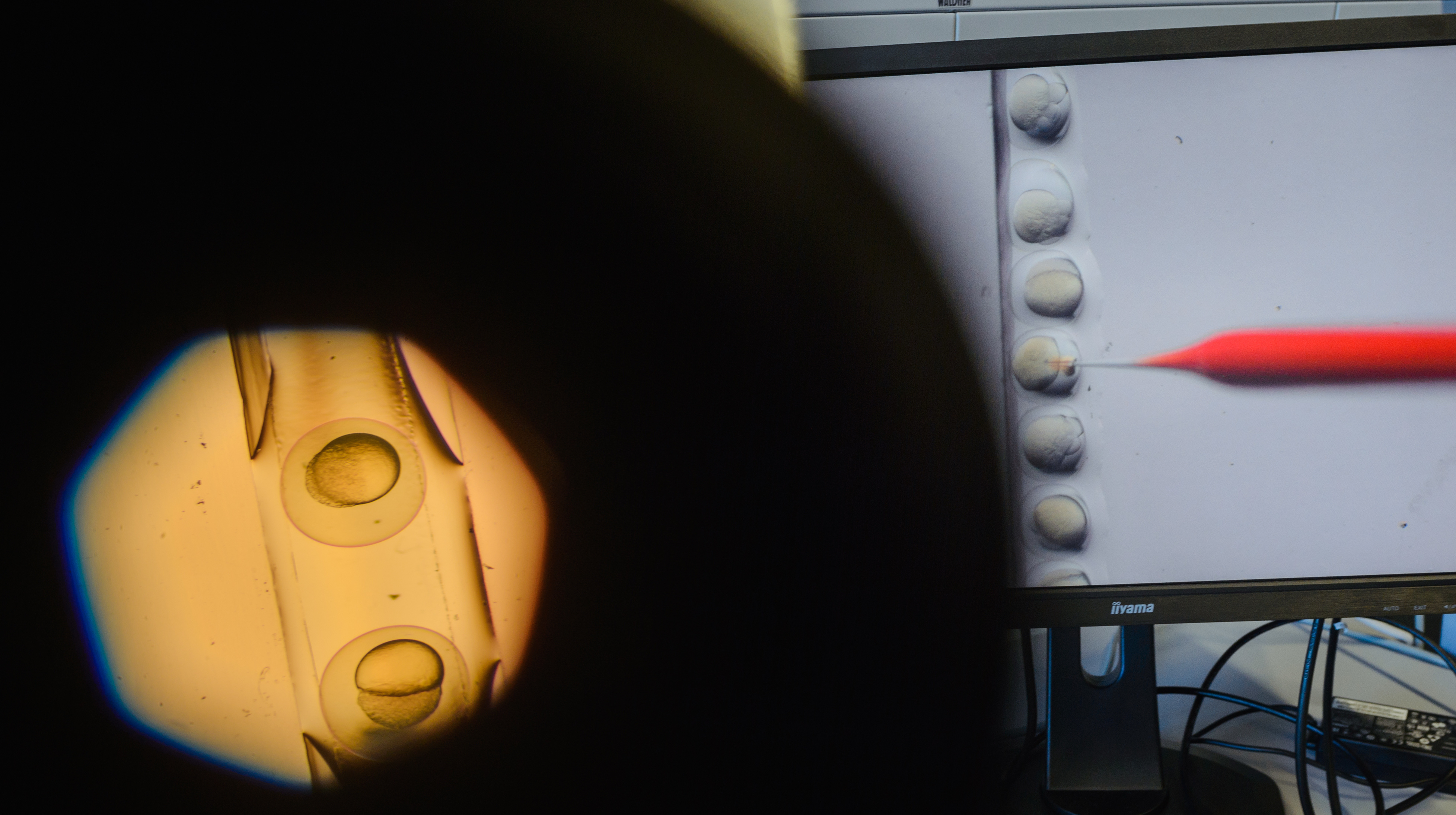
A decade before, a group of regenerative medicine researchers and a 49-year-old with butterfly disease joined forces to test an experimental procedure that showed potential for the rare disease. Their strategy was to combine the regenerative power of stem cells with the corrective power of genetic modification. The researchers harvested skin-producing stem cells from the patient and inserted a healthy anchor protein gene into the cell DNA. They grew the stem cells in a lab until they formed a sheet of genetically modified skin cells, which was then transplanted to a wound about the size of a credit card.
Three-and-a-half months later, the translated cells had fully integrated. The wound was completely healed. More importantly, the area no longer created blisters from slight friction. In that small area, the patient was cured of butterfly disease. So, why don’t all patients with the disease undergo this procedure?
This procedure comes with a significant risk of developing tumors. When the healthy anchor protein gene is inserted into a stem cell’s DNA, there is no way of controlling where in the DNA it will be inserted. Best-case scenario: It doesn’t disrupt any cellular functions. Worst-case scenario: It causes the stem cell to replicate uncontrollably, resulting in a tumor.
The previous patient never developed any tumors, but the doctors only modified very few stem cells for a very small wound. Pat’s wounds were about 150 times bigger. He would need 150 times more genetically modified stem cells, and he would be 150 times more likely to develop a tumor.
So, Pat’s doctors modified the technique of the procedure so it would require fewer stem cells. Or, at least, it would in theory. This modified version of the procedure had never been tested. Three agonizing months after Pat was admitted to the hospital, the procedure began. The doctors removed a thumb-sized segment of non-blistering skin from the left side of Pat’s groin, inserted the gene for a healthy anchor protein, and waited for the cells to grow, hoping the new technique would work.
It did. In just a month, the genetically modified stem cells generated sheets of lab grown skin large enough to begin covering Pat’s wounds. The doctors applied the first sheets to his back and limbs, carefully monitoring for any sign of tissue rejection, which would kill Pat given his critical condition. After one month, the skin had almost completely healed.
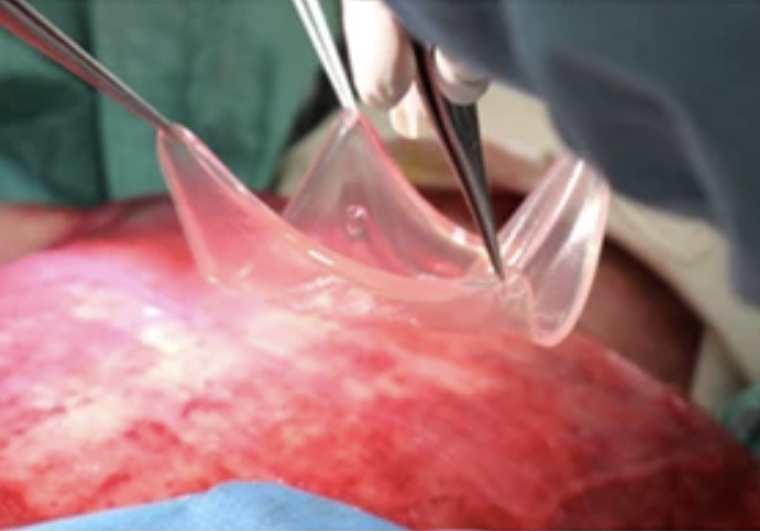
Over the next three months, the doctors treated the rest of Pat’s wounds. In February 2016, eight months after his initial intake, Pat went home.
Act three: The return of Pat
For the past five years, Pat’s doctors have cautiously observed his recovery. It is a massive step in regenerative medicine to replace 80% of the body’s largest organ with genetically modified cells. And massive steps, especially ones made in moments of desperation, are bound to have negative consequences. But, apparently, not this time.
Today, Pat is 13 years old and is the only person in the world to have an organ replaced almost completely by genetically modified cells. Overall, Pat has recovered with no complications. In the areas that didn’t receive genetically modified skin, blisters still develop quite easily. However, the genetically modified skin is healthy and performs all its normal functions (sweating, growing hair, healing from new injuries). There is no evidence of tumors or any other adverse effects, and his functional and emotional quality of life continues to improve.
Pat and his doctors have given some much-needed hope to those besieged by butterfly disease, by paving the way for a combined stem-cell-and-gene-therapy procedure that can be used to cure the disease.