Belly fat: Gut bacteria checks could lead to personalized diets

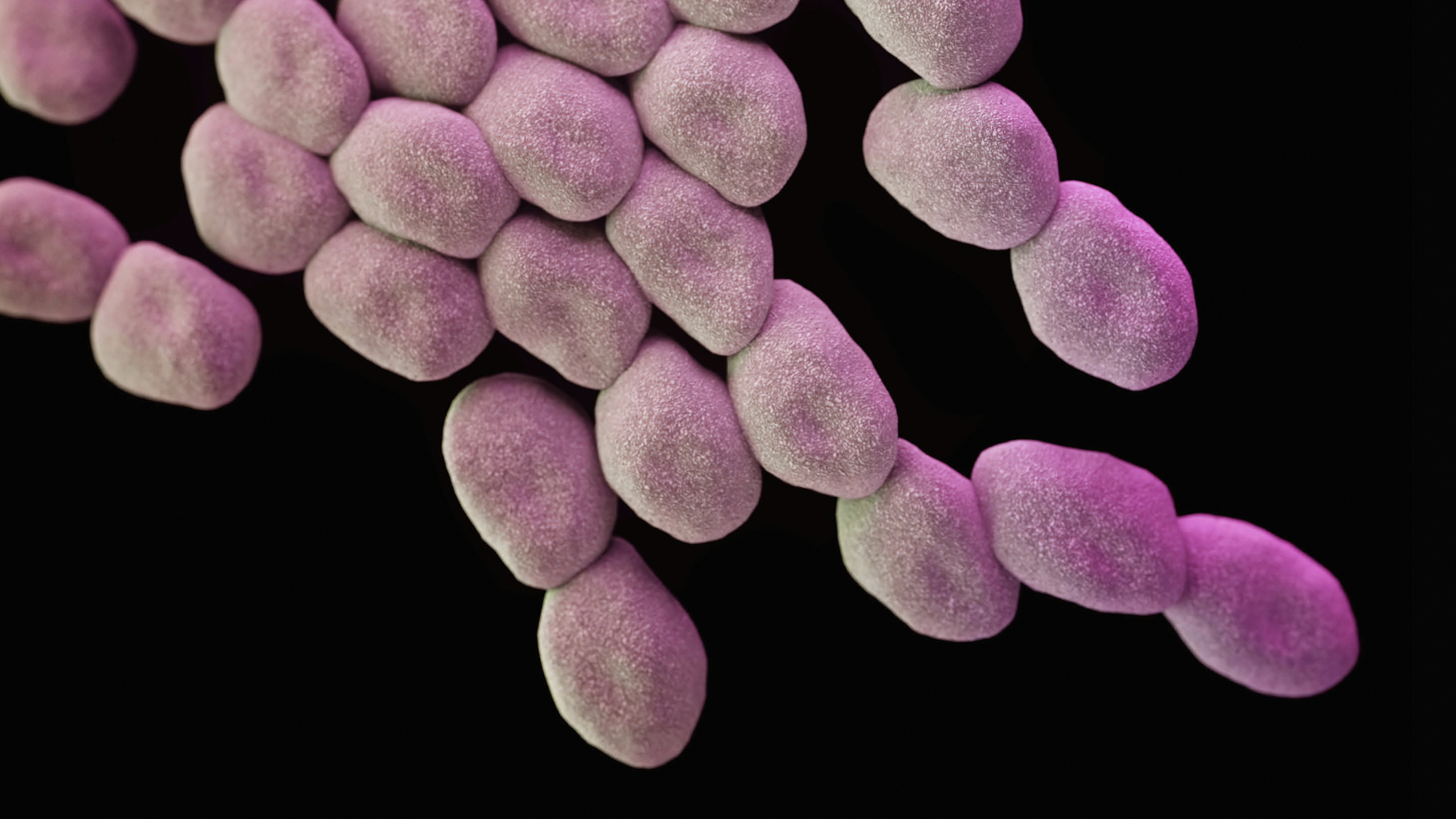
Media for Medical / Getty Images
- New research shows that there’s no one diet that works for everyone.
- Instead, gut bacteria may hold the key to personalized diet plans.
- A future doctor may check gut bacteria to offer diet advice.
Rates of obesity are rising across the globe; a third of the world’s population is now overweight and nearly a fifth is obese.
Public health policy has mainly focused on diet to reverse these rising rates, but the impact of these policies has been limited. The latest science suggests why this strategy is failing: one diet does not fit all. Dietary advice needs to be personalized.
The reason one diet does not suit all may be found in our guts. Our previous research showed that microbes in the digestive track, known as the gut microbiota, are linked to the accumulation of belly fat. Our gut microbiota is mostly determined by what we eat, our lifestyle and our health. So it is difficult to know exactly how food and gut microbes together influence fat accumulation and ultimately disease risk. Our latest study provides new insights into these interactions.
Animal studies have been valuable in showing that gut microbes alone can reduce the build-up of fat, resulting in better health. But translating these findings to humans is difficult, especially considering that we can eat very different foods.
Gut microbes don’t lie
In our study, we aimed to disentangle the effect of gut microbes and diet on the accumulation of belly fat in 1,700 twins from the UK. We found that the composition of the gut microbiota predicts belly fat more accurately than diet alone.
We identified a few specific nutrients and microbes that were bad for us and linked to an increase in belly fat, as well as a few nutrients and many microbes that were good for us and linked to reduced belly fat. The observed link between belly fat and bad nutrients, such as cholesterol, was not affected by the gut microbiota.
In contrast, we found that the gut microbiota plays an important role in the beneficial effect of good nutrients, such as fibre or vitamin E. We show that specific gut bacteria play an important role in linking certain beneficial nutrients to less belly fat. In other words, changes in a person’s diet are less likely to lead to weight loss if the relevant bacteria are not in their gut.
Diet alone did not have a strong impact on the observed links between gut microbes and belly fat, as specific gut bacteria were linked to belly fat accumulation regardless of diet. This confirms what was previously seen in mice, that gut microbiota alone could affect fat accumulation. Our findings also provide further evidence that the human gut microbiota plays an important role in the individualized response to food.
Personalized dietary advice
A limitation of our study was that we analyzed measurements taken at a single point in time. This means that we cannot establish causal links. Also, we focused on reported nutrient intake in the study participants’ diets, but did not assess the effect of total food consumption on its own. Another drawback is that most people misreport what they eat. Researchers are working on improving the way that diet is reported, which should lead to more accurate work in the future.
Our results mean that in the future, you may need to have your gut microbiota checked so that your doctor or dietitian can give you personalized dietary advice. Although bacteria may be partially to blame for the rise in rates of obesity, until we know more it is best to stick to a healthy, varied diet rich in fibre, fruit and vegetables, which in turn may result in a healthier gut microbiota.
Caroline Le Roy, Research Associate in Human Gut Microbiome, King’s College London and Jordana Bell, Senior Lecturer, King’s College London.
This article is republished from The Conversation under a Creative Commons license. Read the original article.