Brain age: High blood pressure makes your brain “older”

- High blood pressure causes a brain to age prematurely.
- “Older” brains are at a higher risk of developing neurological diseases.
- The brain aging effects of blood pressure may begin when an individual is in their 20s.
The clinical relevance of blood pressure is described as far back as 2600 BCE. Maoshing Ni wrote in The Yellow Emperor’s Classic of Medicine (originally titled Huangdi Neijing) that “if too much salt is used for food, the pulse hardens.” Ancient Egyptian physicians in 1550 BCE noted the association between the hardened pulse (i.e., high blood pressure) and heart and brain disease.
While the association between blood pressure and cardiovascular disease is well-studied, scientists are just beginning to scratch the surface of the relationship between blood pressure and neurological disease, such as dementia. And the research is much needed.
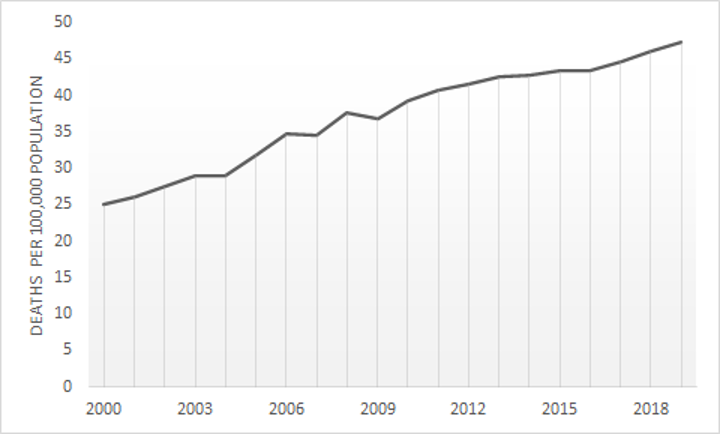
A recent study conducted by the Noncommunicable Disease Risk Factor Collaboration found that the number of adults worldwide who suffer from high blood pressure has doubled from 648 million in 1990 to nearly 1.3 billion in 2019. Additionally, the rate of deaths caused by neurological diseases has increased worldwide, nearly doubling in the U.S. alone between 2000 and 2019.
Elevated blood pressure is associated with micro-damage, which causes the brain to become “older-looking,” and these older-looking brains are more likely to develop neurological diseases. Thus, identifying older-looking brains at key ages could help scientists and physicians determine if someone is at risk for developing a neurological disease in the future. However, until recently, it has remained difficult to determine a brain’s “age” before symptoms start occurring.
This drove an international group of researchers, led by Christian Gaser, to conduct a 12-year study to determine if the brains of individuals with optimal blood pressure stay younger for longer. This question is tricky to answer, as it is difficult to locate micro-damage in the brain, which seemingly occurs randomly. So, scientists first had to answer: How do you find evidence of damage if you don’t know where to look?
Determining your “brain age”
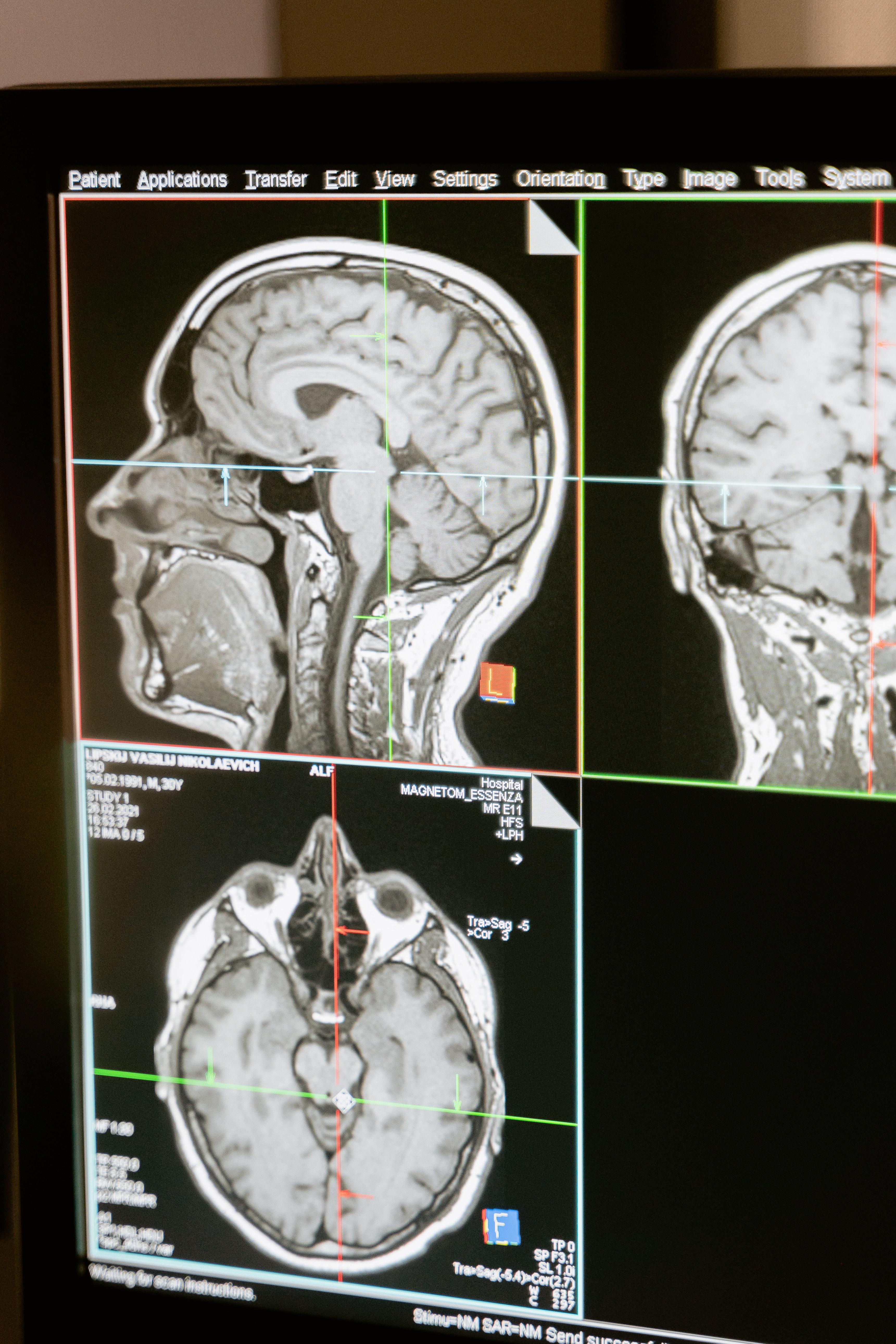
Look everywhere — a simple solution with a difficult execution. Gaser’s team used a machine learning algorithm to analyze 3D brain scans. Called BrainAGE, the algorithm is a novel method that provides researchers with an individual’s “brain age gap estimate” — that is, the gap between an individual’s chronological age and their brain’s functional age.
BrainAGE has become the most widely applied method for evaluating the neurological impact of an individual’s genetics, diseases, environment, and behavior. Lower BrainAGEs have been found in individuals who play music (likely due to increased blood flow, which delivers more nutrients), and higher BrainAGEs have been found in individuals diagnosed with Alzheimer’s.
Gaser’s team sought to use the BrainAGE method to determine if brain damage could be identified in individuals with elevated blood pressure before the onset of a neurological disease. To do so, the BrainAGE algorithm first was fed a couple thousand images of brains of various ages. Next, the program analyzed the brain scans of 686 participants and applied its newly acquired knowledge to predict the functional brain age of each (irrespective of the participant’s actual chronological age).
As predicted, the brains of individuals with optimal blood pressure (110/70 mmHg) appeared the youngest. However, they weren’t just younger than the brains of those with high blood pressure; they also appeared six months younger than the brains of individuals whose blood pressure was toward the high end of the normal range (135/85 mmHg).
These effect sizes may seem trivial — indeed, differences of 6.7 years have been observed between individuals with and without Alzheimer’s disease — but the researchers go on to explain that “an average difference of six months has high relevance as it can serve as an additional risk marker, which, if combined with other risk factors, may be predictive of premature conversion to dementia.”
Concerningly, the researchers also detected brain damage in participants in their 40s. Nicolas Cherbuin, lead author of the paper, said that “we have to assume the effects of elevated blood pressure must build up over many years and could start in their 20s. This means that a young person’s brain is already vulnerable.”