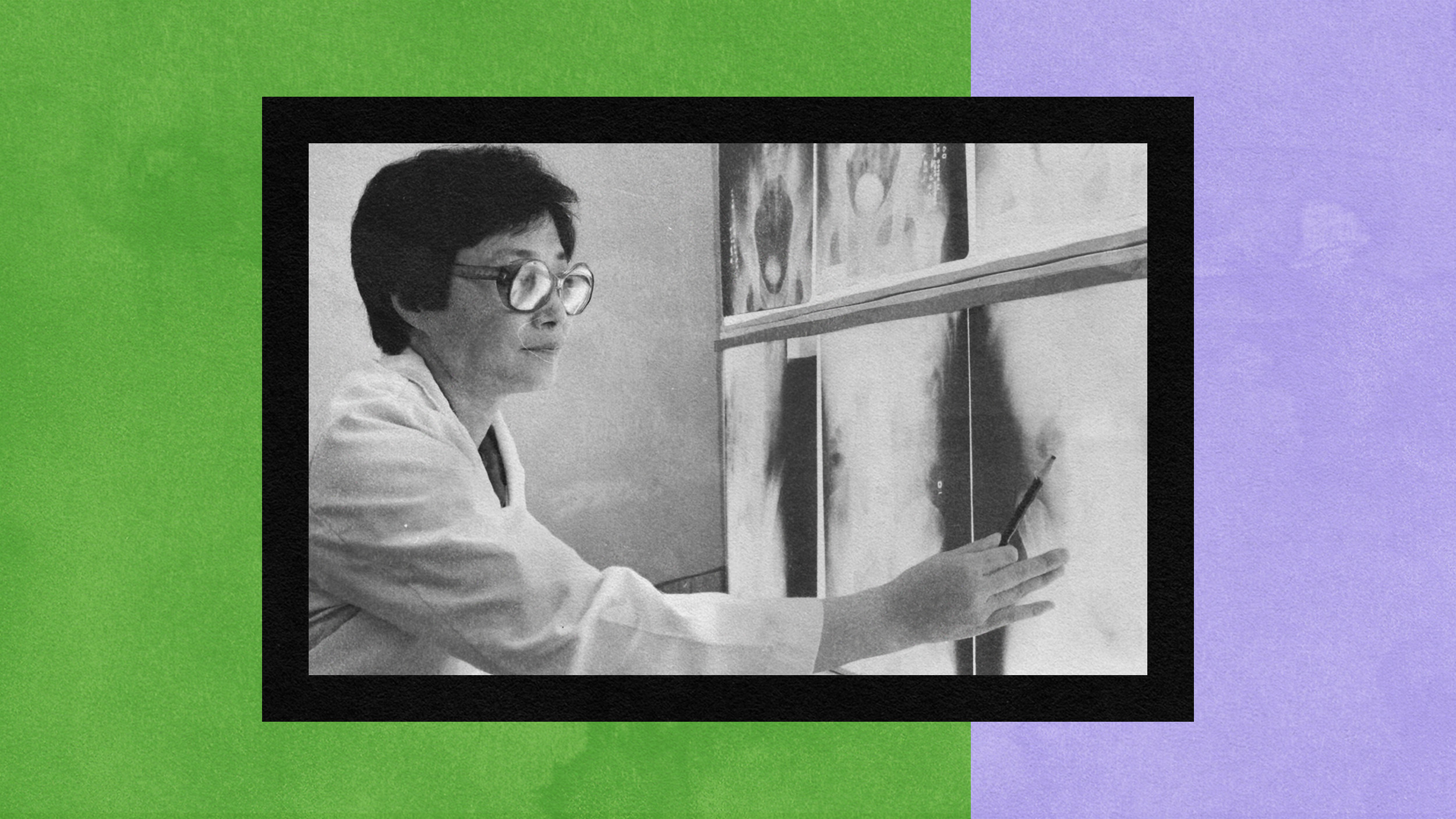
Do You Prefer a Male or Female Doctor? It Can Be a Matter of Life or Death

A recent study published by the Journal of the American Medical Association (JAMA) investigated a rather simple question: Are patient outcomes affected by the gender of your doctor? The answer appears to be yes, though you wouldn’t understand the tenuous nature of this response by the headlines. More surprising than the researchers’ discovery has been the media response.
First, the study. A team led by Yusuke Tsugawa looked at four years of Medicare fee-for-service beneficiaries treated by general internists for a condition that resulted in a hospital visit: a total of 1,583,028 patients for mortality, 1,540,797 for readmission. This represents a random 20 percent sample of total Medicare patient visits during the period from January 1, 2011, to December 31, 2014.
The result? Patients treated by female doctors experienced a lower mortality rate, 11.07 percent versus 11.49 percent, which researchers state is statistically significant at 95 percent confidence interval. Readmissions were also significant at 95 percent, 15.02 versus 15.57 percent.
A few potential reasons cited:
Literature has shown that female physicians may be more likely to adhere to clinical guidelines, provide preventive care more often, use more patient-centered communication, perform as well or better on standardized examinations, and provide more psychosocial counseling to their patients than do their male peers.
This study has significant value in how patients are treated moving forward. Will it increase dialogue between genders about best practices in hospitals? Will specific mechanisms that explain these differences be researched? Are patients going to start requesting female doctors more often? As with all research, it will lead to more research. If lower mortality and readmission are the goals these follow-up questions are necessary.
The Vergejumped on the study a bit differently, with the blaring title, “Patients treated by female doctors less likely to die than patients treated by men, new study shows.” After linking to the research in the first paragraph, the second is a diatribe against gender pay gap and the myth of domestic responsibilities—both important issues, but irrelevant to the topic at hand.
The author goes so far to state the importance of “comparing apples to apples” instead of “apples and oranges,” which is exactly what she does a few paragraphs before. This study was focused on patient outcomes, not longstanding economic issues in the medical field.
Over at The Atlantic the headline reads, “Evidence of the Superiority of Female Doctors.” The author does not wait for the second paragraph to discuss the pay gap—it’s the very first sentence. In fact, this entire article is a platform for equal wages among medical professionals.
What’s interesting is neither article questions the statistical significance of the JAMA study. Ninety-five percent confidence interval is treated as gold standard by most researchers, but a more relevant marker would be at the 99 percent interval. Are the results above statistically significant at this more accurate standard?
There’s no denying that there appears to be a difference; according to the researchers, 32,000 lives could be saved if every doctor is female. While it’s hard to quantify disease in such a way—other factors, such as post-operative care, quality of personal relationships, even the patient’s view from their hospital window or if the facility is equipped with a garden—are all factors.
This is an impossible number to factor in an improbable situation. So we have to work with what is in front of us. Gender pay gap is an important topic in all professions. But taking what is potentially important information for the people that matter most—patients—and co-opting it to make another point takes away from what should be discussed: best practices.
—
Derek’s next book, Whole Motion: Training Your Brain and Body For Optimal Health, will be published on 7/4/17 by Carrel/Skyhorse Publishing. He is based in Los Angeles. Stay in touch on Facebook and Twitter.