Medicaid Will Change, and Almost Certainly for the Better

This week the New England Journal of Medicine published new results from the Oregon Health Study, which randomly selected people for extensions of Medicaid coverage. To anyone who has studied expansions of health coverage in other countries, the results will not have come as a surprise. They may also distract attention from a much more important point about Medicaid.
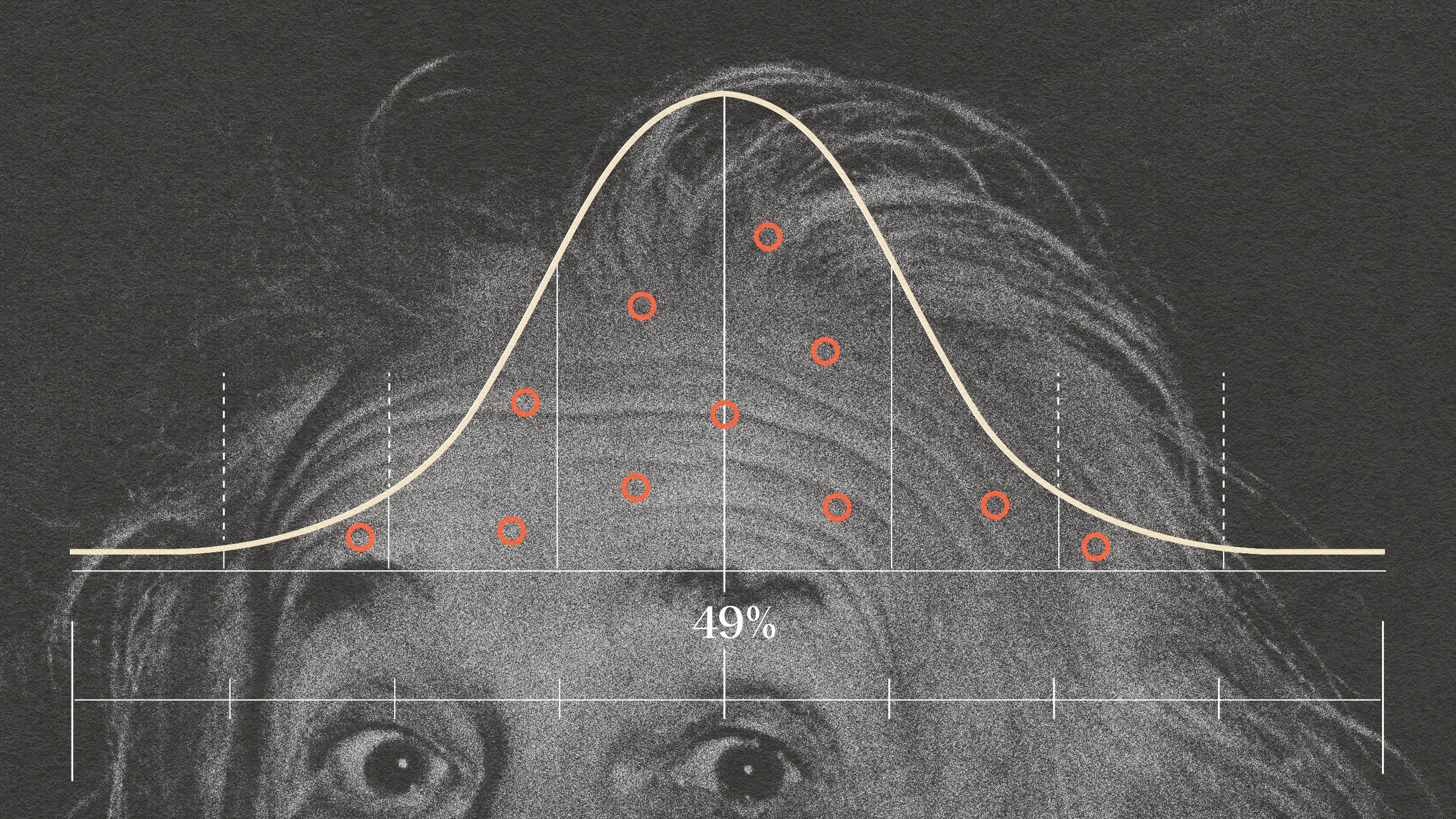
The study, which followed people for two years, found that being covered by Medicaid had little effect on common indicators of health such as blood pressure and cholesterol. This was despite an increase in doctor’s visits and the overall level of health care people received. And it was exactly what health experts have seen in country after country around the world.
The indicators of health in the Oregon study have deep causes, including lifestyle and genetics, that do not change quickly or easily. If you want to see instant effects of health coverage, you have to look at other indicators, like infant mortality: how is a new life affected at its first and most critical moment? In areas like this, where access to health care can make an immediate difference, studies of health coverage typically do find some robust benefits. By contrast, to see results with blood pressure and cholesterol, a study would have to track people for much longer, and perhaps across generations.
That’s why a paper I wrote last year with colleagues from Dalberg and the Council on Foreign Relations focused on the financial benefits of expanding health coverage. We focused on developing countries, but the same findings hold true for poorer Americans. If people have to pay their own medical bills or simply can’t get treatment, a health catastrophe can turn into an economic catastrophe. Coverage by Medicaid instantaneously changes a family’s exposure to financial risk.
The Oregon study did find a significant reduction in financial risk among the new Medicaid enrollees. It also found a decrease in the incidence of depression, which is startlingly prevalent in Medicaid’s target population. Earlier research has suggested links between financial problems and mental health, and also that treatment can make rapid advances against depression. Oregon made valuable gains, and exactly the ones I’d expect to see in a two-year period.
What’s missing from the discussion of the Oregon study is an understanding of how Medicaid might change in the future. Right now, Medicaid is doctors’ least-favorite payer for health care. The reimbursement rates are low, and the patients may feel embattled and under-informed in the health system. If Medicaid expands to cover millions more Americans, it will have a much larger political constituency. With more clout in Washington, Medicaid enrollees will be able to fight against future cuts and for better care the same way Medicare enrollees do.
To sum up, the Oregon Health Study tells us how today’s Medicaid could affect a small number of poor people within two years. Truly finding out how Medicaid might change their lives would take much longer. Moreover, Medicaid would change with time, too – and almost certainly for the better.