2 common drugs may reduce “brain fog” in COVID long-haulers

- COVID long-haulers commonly experience brain fog — a colloquial term for lack of mental clarity, poor focus and concentration, memory problems, and difficulty with multitasking.
- These cognitive process are carried out by the prefrontal cortex, which is sensitive to inflammation and stress caused by COVID.
- Researchers have found that two drugs, guanfacine (an ADHD medication) and N-acetylcysteine (a painkiller overdose medication), clear brain fog symptoms.
COVID long-haulers experience symptoms for weeks or even years after their infection. One of the common complaints among these patients is brain fog — a colloquial term for lack of mental clarity, poor focus and concentration, memory problems, and difficulty with multitasking. Unfortunately, no treatment options are currently approved for the condition. Luckily, Yale researchers have discovered a drug combination that can mitigate or even eliminate brain fog. The best part is these drugs are already available to patients.
A foggy prefrontal cortex
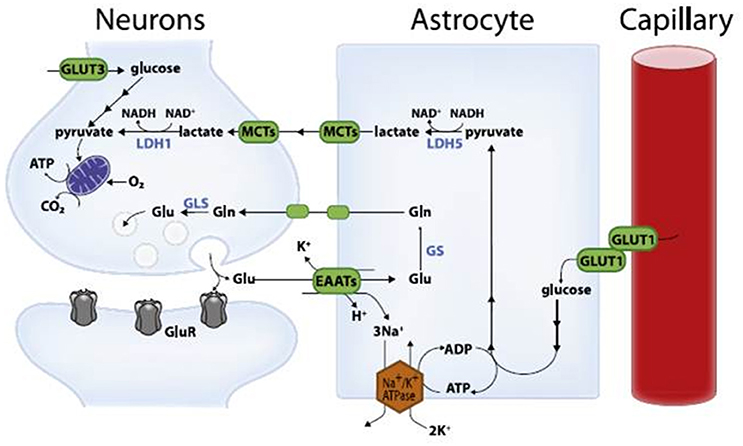
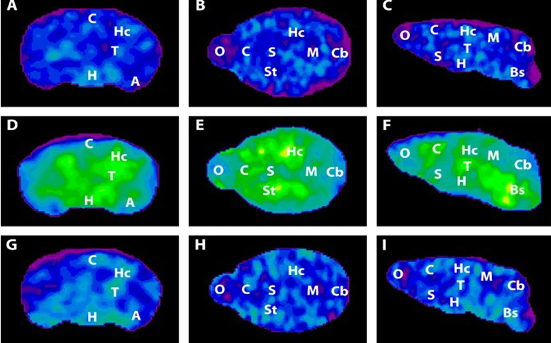
Executive functioning, working memory, and attention regulation are carried out by a recently evolved area in the brain called the prefrontal cortex. The neurons in this region form highly interconnected, circular neural circuits, which help keep information “in focus” without requiring external stimulation. Unfortunately, these circuits are also vulnerable to inflammation and stress.
“The circuits that generate higher cognitive function have very special molecular needs because they’re having to create neural activity without any sensory stimulation — abstract thoughts and memories, for example,” said Amy Arnsten, a professor of neuroscience and psychology who has spent decades studying the circuits behind cognition.
According to Arnsten, COVID can cause inflammation that interferes with the prefrontal cortex’s molecular needs and disrupts delicate neural connections. Therefore, drugs that restore the circuit could help alleviate brain fog.
COVID and concussions
In the early 2000s, Arnsten’s lab developed guanfacine, a compound that strengthens prefrontal cortex connections, protects against inflammation and stress, and improves cognitive function. The drug was approved by the U.S. Food and Drug Administration (FDA) for the treatment of ADHD in 2009, but clinical neuroscientists, such as Arman Fesharaki-Zadeh, also use it off-label to treat other conditions associated with prefrontal cortex dysfunction, such as traumatic brain injury and PTSD.
Fesharaki-Zadeh faced his first long COVID case in June 2020, and he recognized the overlap between the brain fog his patient was facing and the symptoms in his traumatic brain injury patients. For years, he and his colleagues had been treating these patients’ cognitive symptoms with a combination of guanfacine and N-acetylcysteine (NAC), a robust antioxidant and anti-inflammatory agent that is FDA-approved for treating acetaminophen overdose. So, Fesharaki-Zadeh wondered if the drug combination could also successfully treat COVID-related brain fog.
“I had the idea of approaching the treatment from two different perspectives — modifying the pro-inflammatory, pro-oxidation pathway with NAC, and treating the post-COVID neurocognitive sequelae impacting executive functioning with guanfacine,” he says. “We wanted to attack this using a multi-model approach that took advantage of the synergistic relationship between NAC and guanfacine.”
Clearing the fog
Fesharaki-Zadeh and Arnsten followed eight patients who were prescribed guanfacine and NAC for long-COVID cognitive complaints starting in December 2020. The patients described “brain fog” as significant difficulties in executive functions such as multi-tasking, focus, and concentration. All eight patients reported benefits, and some reported that their brain fog had completely disappeared.
The lack of a placebo group means that these results must interpreted with extreme caution. But there is anecdotal evidence to suggest that the drugs were working as intended.
One of the patients was a nurse on a medical floor who, after contracting COVID, felt overwhelmed at work and had to decrease her caseload. Following treatment, the nurse experienced significant benefits in her working memory, executive functioning, and cognitive processing speed. She reported being able to fluidly manage her tasks at work and return to a normal caseload. Her cardiologist had briefly stopped the guanfacine due to an episode of low blood pressure. While stopping the guanfacine, she experienced a significant worsening of her cognitive functioning and concentration. After her blood pressure returned to normal, she resumed the guanfacine regimen, and symptoms again improved.
Guanfacine and NAC are available now
To reiterate, a placebo-controlled trial is absolutely mandatory to determine if this treatment actually worked. Indeed, the researchers hope that their case study will lead to the funding of placebo-controlled clinical trials involving a larger cohort of patients. But such studies will take years to complete.
Fortunately, because guanfacine and NAC are readily available (the latter is over-the-counter), long-haulers who are debilitated by their symptoms can talk to their physicians about a prescription.*
The researchers also hope that this regimen can be helpful in other groups of patients. COVID is not the only disease to cause brain fog. For example, patients with Lyme disease, myalgic encephalomyelitis, and multiple sclerosis can also experience debilitating cognitive deficits. Indeed, Fesharaki-Zadeh has already seen cognitive benefits while treating Lyme disease and multiple sclerosis patients.
“I just feel so grateful for my collaboration with Amy Arnsten and that my understanding of traumatic brain injury could be helpful,” says Fesharaki-Zadeh. “Our success was a combination of having the right knowledge at the right place and time while working with the right people.”
*Editor’s note (April 2, 2023 @ 5:45 am ET): A previous version of this article stated that guanfacine was available over-the-counter. This is incorrect. It requires a prescription. Sorry.