- Benjamin Chan is a Yale researcher collecting bacteriophages (bacteria-destroying viruses) in hopes of treating superbugs. Paige is a cystic fibrosis patient in Texas with an antibiotic-resistant pseudomonas infection which has further reduced her already limited lung capacity, and Ben’s therapy is her last resort.
- While superbugs have evolved resistance to our most powerful antibiotics, the phages Ben has found in water samples around the world could be capable of knocking them out.
- In this documentary, we follow Ben as he travels from his laboratory in New Haven to Lubbock, Texas to deliver the treatment – and meet Paige as she shows us what life is like before and after this experimental phage therapy.
- This episode was originally created and shared by Freethink.
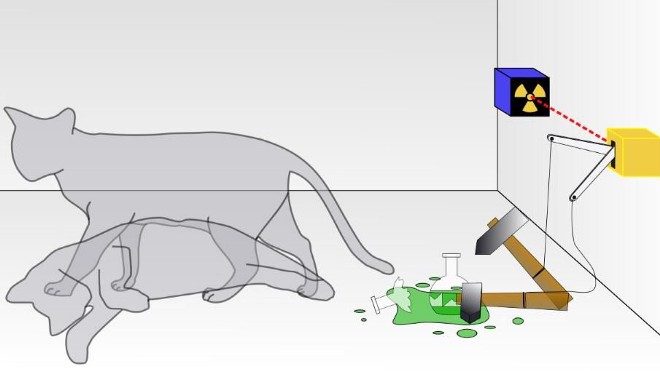
BENJAMIN CHAN: Bacteriophages are the most numerous replicating entity on the planet. There are more phages than there are stars in the universe. Every drop of sea water has 10 million bacteriophages in it. Bacteriophages are a virus that's basically pathogens of a pathogen. We're at a point in time now where the antibiotics that we've used for decades have increasingly become less effective at treating infections. If there is a tool that we could use that could help someone, then of course we should try and pursue it.
PAIGE ROGERS: You guys have a merry Christmas. Cystic fibrosis is what you would refer to as an invisible disease because on the outside I look completely fine, but that doesn't mean that's how it is on the inside. Cystic fibrosis basically covers the entire inside of my body in mucous. That makes it where it messes up the lungs, the pancreas, the liver, pretty much everything. Yeah, I feel so tired I can't function. I'm like ugh.
ADAOBI KANU: Are you like, um, are you feeling achy? Or is it just this overall...
ROGERS: Just tired and coughing.
KANU: Okay, alright, sweetheart, we're gonna have you come over here to do the lung test. If you're ready. Blow, blow, blow, blow, blow, blow, blow, blow, blow. Deep breath in. 69 percent. Mkay, alright.
ROGERS: The higher your lung function is, the better your life expectancy is. And actually on the paper, it will say like this is the lung health of a 67 year old. So I'm 22, but it shows on there 67 years old. I wanna be a mom one day. To think maybe one day I can go nine months without being on all those antibiotics. Then I would have nine months where my baby could grow in a normal body. My best case scenario for phages is to at least get my lung function to 85 to 90.I would be so happy.
CHAN: Okay, so here's my fridge full of all my water samples and some phages from all over the world, places I've visited to sample. This is sewage from a town in Mexico called Cuatro Ciénegas. From here there's a pig farm, here in Connecticut. These are from Uganda and Kenya. I have phages that we use to for Paige, here.
NARRATOR: Where do they come from?
CHAN: So New Haven, Lyme, Connecticut and one from East Africa, from in the Congo. Boom. So as you can see in the tube here on the left, it's Paige's bacteria alone, okay. And the one on the right is uh, Paige's bacteria plus bacteriophage. And you can see it's really turbid or cloudy, since the bacteria is growing. And in this tube here it's very clear, which means that phages killed bacteria. So from here, all we gotta do is clean up the prep, concentrate the phages and then we can ship it off to Paige.
ROGERS: On a daily basis I spend probably about four hours just maintaining my health.
NARRATOR: And so how long do you have to be wearing your vest?
ROGERS: Thirty minutes, it's on the highest setting right now, and even though it works, it still doesn't get everything.
ROGERS’ MOTHER: So what time do you have to be at the hospital tomorrow?
ROGERS: I have not been informed, about anything.
ROGERS’ PARTNER: Well from what Dr. Chan said, it seems like a pretty promising method of treatment.
ROGERS: Yeah, like, I'm excited for the phages 'cause I just really feel like they're gonna work for sure. But I'm really nervous as well because it's my last option. Yeah, 'cause antibiotics don't work at all anymore. So I really need these to work.
CHAN: Little bit nervous but I think I'm prepared. I hope I'm prepared. We're at the Dallas airport right now, and we're about to catch a flight to Lubbock, Texas so we can treat, um, Paige. Tomorrow morning I'm most looking forward to meeting Paige actually, and then obviously, getting passed the treatment, um. It's really just gonna be super simple.
ROGERS: About three years ago, it was time to treat the pseudomonas and I did a two week round of antibiotics and it didn't work. My lung function didn't go up from it, and my pseudomonas didn't go away. I couldn't even do things like take a shower by myself. Whenever I lifted my arms up to wash my hair, I couldn't breathe, I would feel like I wanted to cry. I needed help with absolutely everything. To think that without the phages, that could be my normal life is extremely scary.
CORY ROGERS: We're uh, fixin to do phages for Paige, for the first time. Since Dr. Canoe actually set everything in motion I guess it's only been seven months but, it seems a lot younger, so yeah. It's been a long time coming.
NURSE: So we just want to make sure that you are aware this is experimental, it's not a proven scientific thing , okay?
ROGERS: This could be a game changer for Paige, ya know? This could be the key to her living a normal life. Having children. Uh, going on to do the things, you know, she's always wanted to do. She could go far, but this disease has held her back.
ROGERS: I discovered phages actually by hearing about it from my dad.
KANU: Mr. Rogers brought this up to me and, after finding several articles on bacteriophage, I was able to share this information with Dr. Chan, which he very quickly came up with a cocktail of bacteriophage for her.
ROGERS: I don't know if it will all fit in there.
CHAN: 10 mils. It's a little terrifying to think that like, something that I made was going to be used as medication. It's not like it was made somewhere else and I was just delivering it, like, I made that.
ROGERS: I feel really excited especially since it's almost done and there aren't any side effects that have gone wrong.
ROGERS: I have to miss out on a lot as it is, you know. But there's times you just gotta be there, you know. This is definitely one of them.
ROGERS: It still doesn't feel real. I'm hoping in five years I can look back at this and be like, whoa, wasn't that crazy that was my last option and look at me now, with lung function in the 90's, living life normally.
ROGERS: Anyone who knows me knows I like my makeup. I get up, I put my makeup on even if I'm not going anywhere. I literally, in February, went two weeks without putting on makeup, laying on the couch in my pajamas so I felt like, man I don't know if this is working. But March came and I was like, wow. I thought, uh, it's making me worse. But no, it's definitely making me better.
KANU: Blow, blow, blow, blow, blow, blow, blow, blow, blow. Deep breath in. The air in one second was 79% so, we would call this stable.
ROGERS: My lung function really isn't that much better, yet it feels so much different.
CHAN: You know, within ten days after we started giving her bacteriophages to treat her lung infection, we found that the bacteria that was growing in her lungs had reverted to being drug sensitive again.
ROGERS: I needed the phages to make me where I wasn't antibiotic resist anymore. Now that I can use the IV's, I use that to get rid of the pseudomonas. Whenever Dr. Canoe first showed me how sensitive my pseudomonas was to all these antibiotics, I didn't care who I was around, I just started bawling.
ROGERS: Well she's got a lot more energy. You see her wanting to do things. You can just tell she feels better.
ROGERS: Before if all I could do was lay on the couch and stay inside, how could I get a good job, how could I be a mother? But now there's hope, because I have energy. Casey even said that he can see a difference in my quality of life and how I've been acting. He loves it when I go to the gun range with him, but I never would, so he's been excited, because we're able to do more together now.
CHAN: When she volunteered for this treatment is was huge for the CF community, the scientific community, and there's a lot of people that could really benefit, I think, from the results of this.
ROGERS: To be completely honest, I had no idea what the phages were going to do. But now there's times I think about it at night and I still just cry, 'cause I'm so happy. Like, to think, okay we got this under control. Like, life's good.
ROGERS: I don't like your gun.
ROGERS: Huh?
ROGERS: I don't like your gun.