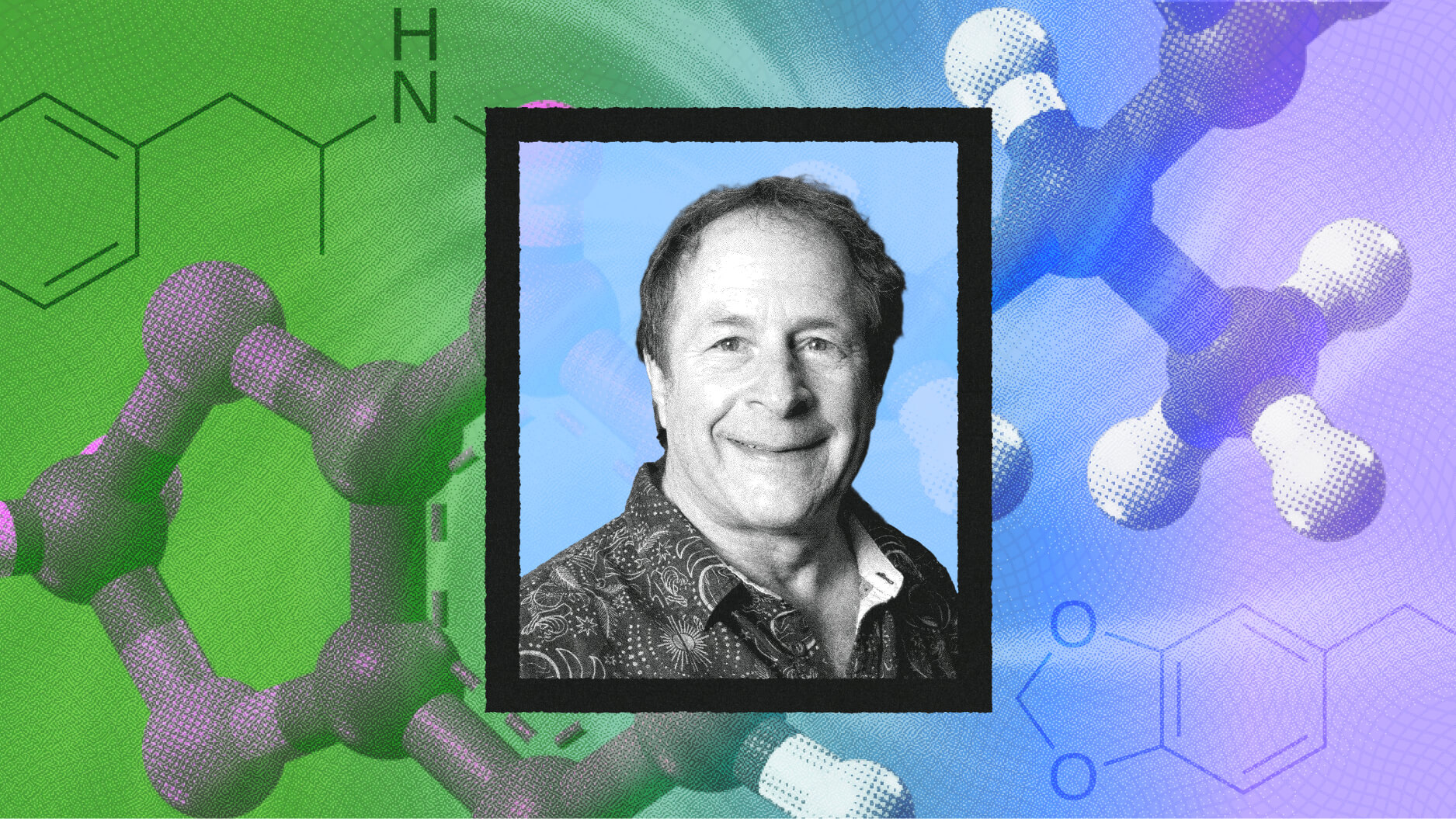
Dr. Q says that, as a neurosurgeon, he has incredible access to the brain through surgery, which proves invaluable in the laboratory where he can help get to the root causes of diseases. But, he also warns the public that we are at a crisis point when it comes to supporting scientific research in the United States.
Question: How do you describe your scientific research?
Alfredo Quinones-Hinojosa: Well the best way that I can describe what I do as a scientist is the following. We have an opportunity, a wonderful opportunity. The opportunity is that my patients, our patients, allow us to go into the operating room every day. No one has more access to the human brain and the human central nervous system than we do as neurosurgeons. The reality is that many times to make a diagnosis you just need a small microscopic amounts of tissue. And many times the rest of the tissue just ends up in the biomedical waste, and we never do anything with it. And I decided that I want to go back to the basics.
And what I do is very simple. I use that tissue; that human tissue that otherwise would be absolutely discarded, I use it to take it back to the laboratory. I'm given that privilege by my patients. In the laboratory what we do is also complex, but simple in some ways. We're trying to understand whether or not within this tissue there are cells that have the ability to initiate brain cancer. We're trying to get to the root of the problem. So far what we have done with brain cancer is try to cure it.
The reality is that we don't even know how it starts. So what we try to do in our laboratory is try to understand how it may possibly start, and whether or not there is anything that we can do to prevent these little cells from migrating away and creating more havoc in the brain. And we do that by using models that are alive in animals and by using the small dishes where we can actually grow cells and see their behavior, see how they move, see how they grow, and see whether or not we can learn from that.
Question: How do you balance life in the operating room and the lab?
Alfredo Quinones-Hinojosa: The balance is not simple, it's actually quite complex. And the way it works is the following, in my experience, is you have to find a line of work that matches what you do in the laboratory and what you do in the operating room. In my case I am a brain surgeon and a spine surgeon, and I mainly specialize in brain tumors type of disease. Why? Because they actually fit exactly what I study in the laboratory.
So every time I am in the operating room, as an extension I am being part of my laboratory by collecting tissue, by collecting fluid, by interacting with my patients, by exploring and studying the disease which I study in the laboratory. So that's part of what I do. In general, it's not a simple recipe. It varies day to day, it varies week by week, it varies month by month. But the most important thing is that you have to find the time to do both, and if those two careers do not match, then it's virtually impossible to make it happen.
Question: What should the public understand about your research on the brain?
Alfredo Quinones-Hinojosa: What the public needs to know is undoubtedly that we are at a crisis. We spend a fair amount of money on many things in life, in our society, and unfortunately not enough on research. I have been extremely privileged that our work is being supported from several organizations, including the National Institute of Health, the Howard Hughes Medical Institution, the American Association of Neurological Surgeons, the American College of Surgeons, the Children's Cancer Foundation, the Robert Wood Johnson Foundation, the Maryland Stem Cell Research Foundation, and some other organizations that have been extremely wonderful in their support of our work. However, if you think about it, all those are small, little grants.
Although they're indispensable and they're extremely crucial for our work, they don't amount to very much at the end of the day. And to be able to do what we do, to be able to pay the salary of my post-docs, to be able to pay the space in which we do laboratory research, to be able to pay for all the resources and all the personnel that it takes to run such a laboratory is a fair amount of money. And the reality is that not a lot of people, and not a lot of investigators, are as lucky as I have been in my life to be able to obtain these grants. So there is a lot of investigators that are struggling to obtain more funding for their laboratories.
So what we need to do, and what the public needs to know, is that for us to be able to find a cure for brain cancer, we need to put those dollars, we need to put those resources to work. I know, based on what I do, and based on what other people have done-- and I stand on the shoulders of giants and I can do this because a lot of people ahead of me have done it for many years-- I know that the cure for brain cancer is not going to be won in the operating room. For me the operating room is a crucial part of my laboratory, so it's indispensable as well, but I know we're not going to find that cure in the operating room. That cure has to be found back there, in the laboratory, at the bench site every day, doing it over and over.
Recorded on: July 2, 2008