Scientists find a marker for schizophrenia in human hair

Photo by Mohamed Nohassi on Unsplash
- Schizophrenia can be difficult to diagnose early, which is why it’s important to identify physical markers that appear in schizophrenics but not the healthy population.
- To determine this, researchers examined mice with schizophrenia-like symptoms and compared them to a healthy group. They found that the mice with schizophrenia-like symptoms had elevated levels of MPST, an enzyme that produces hydrogen sulfide.
- Not only does this provide a biomarker for schizophrenia, but it also suggests that schizophrenia may come about due to what the researchers called “sulfide stress.”
Schizophrenia is a multifaceted disease, and its signs and symptoms are multifaceted as well. Like all behavioral diseases, it can be difficult to detect, especially early on. But recent research published in EMBO Molecular Medicine found a potentially game-changing means of detecting schizophrenia through hair samples.
The researchers began by investigating another diagnostic test for schizophrenia. Healthy mammals tend to exhibit something called the prepulse inhibition response, or PPI. Everybody tends to jump when they’ve been startled by, say, a loud noise, but if that noise is preceded by another, quieter noise (the prepulse), they’ll be less startled by the second sound. That’s the PPI response. Schizophrenics, however, tend to have a lower PPI response: they react just as suddenly to a loud noise as they do to one that’s been “previewed” by a quieter sound.
The researchers wanted to study the different physical markers between heathy individuals and schizophrenics, so they studied the proteins found in a strain of mice that frequently exhibited symptoms of schizophrenia, including a lowered PPI. What they discovered was that mice with low PPI tended to have higher levels of an enzyme called MPST. This enzyme produces hydrogen sulfide, also highly present throughout the mice.
“Nobody has ever thought about a causal link between hydrogen sulfide and schizophrenia,” said research lead Takeo Toshikawa. To ensure that the hydrogen sulfide was responsible for these behavioral changes, Toshikawa and colleagues knocked out the gene for MPST in the mice. Without this gene, mice exhibited significantly higher PPI than mice who still had the gene for MPST, who still had hydrogen sulfide circulating throughout their bodies as a result. “Once we discovered this, we had to figure out how it happens and if these findings in mice would hold true for people with schizophrenia,” said Toshikawa.
Schizophrenia – causes, symptoms, diagnosis, treatment & pathology
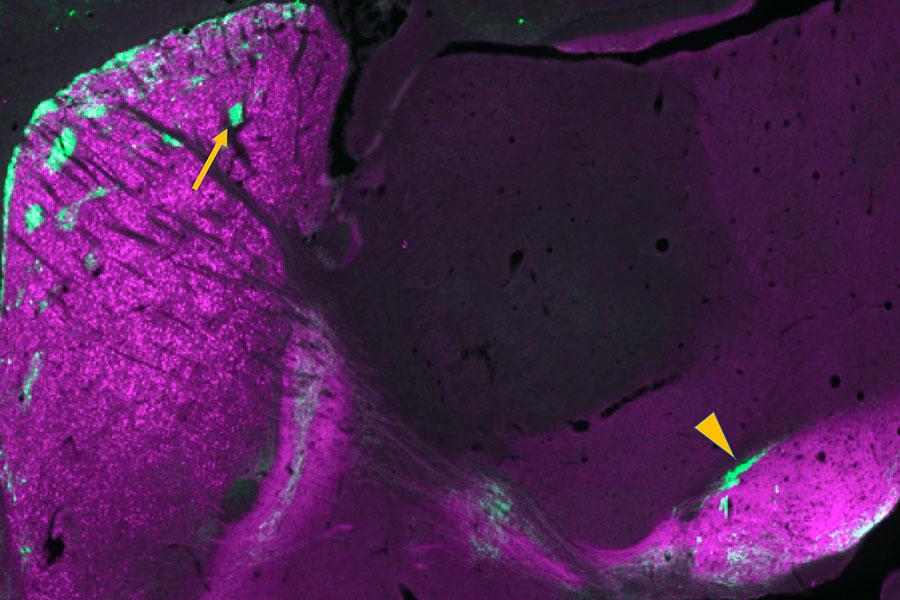
The research team then moved onto examining the brains of deceased schizophrenics and healthy individuals. All of the schizophrenic brains had more MPST present in their cells, and, intriguingly, higher levels of MPST were associated with worse schizophrenic symptoms. What’s more, when the researchers tested the hair follicles of living subjects with schizophrenia, they found that the presence of elevated MPST was a fairly reliable marker for schizophrenia. However, this was not true for every individual with schizophrenia, indicating that whatever role MPST and hydrogen sulfide plays in schizophrenia, it wasn’t the only route to the disease.
Finding out the nature of that role was the researchers’ next task. The research team knew that hydrogen sulfide helped reduce oxidative stress and neuroinflammation in the body. Prior research had also uncovered a correlation between inflammatory events that occurred before and just after birth and schizophrenia. Furthermore, high levels of hydrogen sulfide circulating through the body were related to a greater risk for ulcerative colitis and a lower risk for rheumatoid arthritis — schizophrenics are both more likely to have ulcerative colitis and less likely to have rheumatoid arthritis as well.
Taken together, these previous findings all seemed to point towards hydrogen sulfide possibly playing a part schizophrenia’s cause. To test this, the researchers turned once again to mice. They injected pregnant mice with polyinosinic:polycytidylic acid (poly-I:C), a compound that mimics viral infections and stimulates the immune system. When the pregnant mice gave birth and those offspring grew to adulthood, their brains featured significantly higher expression of genes associated with antioxidant and anti-inflammatory production, including hydrogen sulfide.
This led the researchers to conclude that early inflammatory events cause changes in the genome such that the body produces higher levels of hydrogen sulfide. They argued that this elevation in hydrogen sulfide causes what they term “sulfide stress,” which may contribute to the neurology of schizophrenics.
More research will be needed to confirm or deny this theory, but it does help fill in some of the gaps of our understanding of schizophrenia. In recent years, more and more evidence has been accumulating to suggest that neuroinflammation during a child’s development contributes to or even causes schizophrenia. Knowing for certain whether that’s the case is still a long way off, but if it is true, then sulfide stress may very well play a role.