Do you have a cold, the flu, or COVID-19?
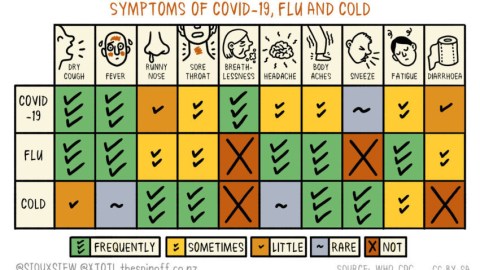
Credit: Siouxsie Wiles and Toby Morris, The Spinoff
- Differences in symptoms exist between a cold, the flu and coronavirus.
- The CDC issued specific recommendations about what to do if you’re sick and when to get tested.
- Calling the doctor is important if you feel sick or have questions.
How do you know you have coronavirus?
With so much misinformation flying around, it’s important to understand the differences in the symptoms between COVID-19 (the infamous coronavirus), the regular flu, and a cold. A number of symptoms overlap between these three ailments, often making it hard at first to figure out which one you might have.
In particular, all three share dry coughing, a runny nose, a sore throat, body aches, and fatigue. But a fever is not a frequent symptom of colds, while it’s a feature of the flu and coronavirus infections, as are diarrhea and headaches.
If you find yourself sneezing, that’s not as common for the coronavirus or the flu, but would strike you if you had a cold.
The Spinoff, a media portal from New Zealand, made a handy chart, featured above, which summarizes the variations.
Breathlessness and respiratory trouble are the hallmarks of COVID-19. These and symptoms like cough and fever tend to appear from 2 to 14 days after exposure to the virus.
Another symptom of coronavirus that has been gaining attention is the sudden loss of taste and smell.
Based on a rising number of cases around the world, the American Academy of Otolaryngology – Head and Neck Surgery and ENT UK both released warnings that some patients tested positive for coronavirus with only the changed sense taste or smell being the symptom.
How to get tested
The CDC maintains that not everyone needs to get tested, especially as there’s been a lasting shortage of tests, which has caused havoc in medical facilities throughout the country and likely damaged containment efforts.
Another reason to not get tested: Most people who get coronavirus generally develop mild symptoms and can get better at home.
There’s also no special treatment currently available for coronavirus, even if some medicines are being closely studied.
Furthermore, as CDC writes in bold on its page “decisions about testing are at the discretion of state and local health departments and/or individual clinicians.”
If you believe your symptoms are getting worse and merit testing, you should try giving a call to your state or local health department or your doctor. The doctor would be the one to recommend your case to the state and local department to try to get you tested.
What to do if you’re sick?
If you do get sick or think you’re falling sick, the CDC recommends some steps to protect both you and the community at large.
* Stay at home
Overall, you should stay at home unless you need to get medical care. This is both for your health and for the safety of everyone else, who might be infected if you were to go out.
You would also be more comfortable at home.
* While at home, you should still try to stay away from other inhabitants there and seek isolation, limiting your interaction with pets and animals to not get them sick either.
* You should also try to reduce stress, as anxiety about the illness can cause you additional ill health whether you have coronavirus or not. The CDC would like for people to take breaks from watching the news and being on social media, taking better care of their bodies, unwinding and connecting with others.
* Call your doctor before you go to get medical care. Especially if you’re feeling worse.
* Avoid public transportation so you don’t spread the disease.
* If you’re outside, wear a face mask if you are sick. That way you won’t infect people.
* You should also continue practicing good hygiene: wash your hands often; avoid touching your eyes, nose and mouth; cover your mouth while you cough or sneeze, ideally into a tissue or the crook of your elbow, not your hand; and clean and disinfect high-traffic surfaces in your house.
10 things you can do to manage COVID-19 at home
When to go to the doctor?
The CDC recommends that if you develop warning signs for COVID-19, you should consider it an emergency and look for medical attention right away. Remember to call ahead.
The emergency warning signs are:
- Trouble breathing
- Persistent pain or pressure in the chest
- New confusion or inability to arouse
- Bluish lips or face