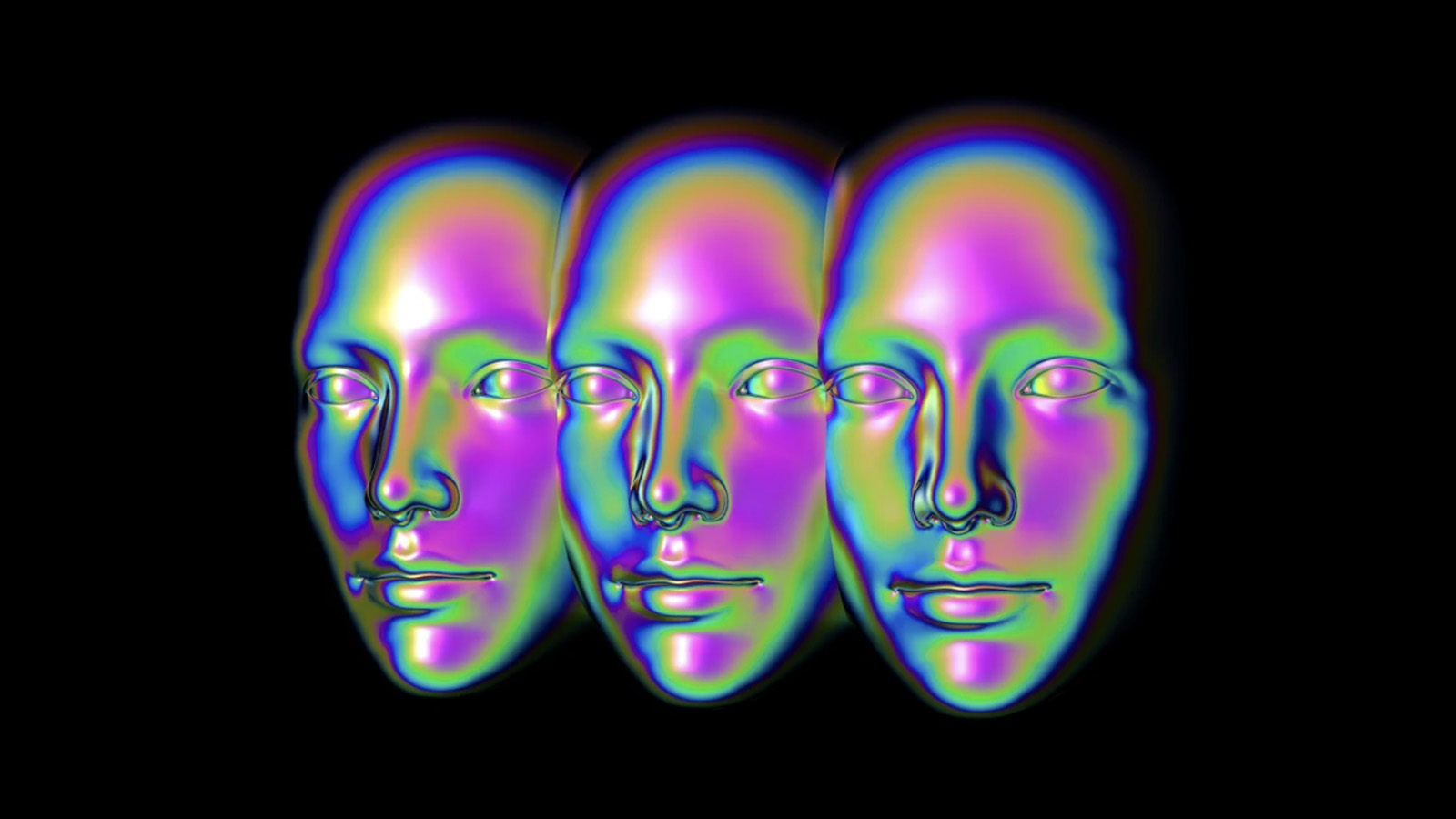
What happens to a person’s sense of self after a face transplant?

- The first study of self-recognition in a face transplant patient shows that the mental representation of the self is preserved but gradually incorporates the new face.
- The findings suggest that the brain mechanisms underlying self-face recognition are malleable.
- Individual responses to face transplant are, however, likely to vary widely.
Faces are crucial for social interaction and our sense of individuality. We recognize others primarily by their faces, and the ability to recognize one’s own face in the mirror is used as a test of self-awareness in children and animals.
Faces are so special that the brain contains areas and networks that are believed to be specialized for processing them. Viewing other people’s faces activates a small region of the visual pathway known as the fusiform face area, whereas self-face recognition activates a much wider distributed network.
The question of what happens to one’s sense of self-identity after acquiring a new face remained a philosophical thought experiment until 2005, when a surgical team in France performed the first partial face transplant. Since then, nearly 50 such procedures have been performed on patients whose faces were disfigured by injury or disease.
Now a team of psychologists led by Ruben Azevedo of the University of Kent reports the first longitudinal study of how an individual’s self-face recognition changed before, during, and after receiving a face transplant.
A new face
The patient was a 25-year-old man who sustained severe facial injuries in 2016 and underwent several surgical procedures to have part of his face and his entire jaw replaced when a suitable brain-dead donor was identified some 18 months later. Azevedo and his colleagues assessed his self-recognition eight months and two months before his operation, as well as three times after it, with behavioral tests and brain scans.
At each time point, the researchers showed the patient photographs of his own face before the injury, after the injury, and after the transplant, each of which was “morphed” to varying degrees with other, familiar faces, and asked him to indicate whether each one looked more like him or the other person. They also used functional magnetic resonance imaging to scan the patient’s brain and determine the extent to which each photograph activated the self-face recognition network.
The behavioral tests showed that the patient was initially biased toward recognizing his pre-injury face. That is, only a small percentage of his own face needed to be present in the morphed image in order for him to recognize it as “self.” But for morphed images of his injured face, the patient only identified those containing a larger percentage of his disfigured face as “self.”
The brain scans showed increased activity in response to images of the patient’s pre- and post-injury faces, but some components of the self-face recognition network were activated more strongly by the pre-injury face. This suggests that the patient’s mental representation of his pre-injury self-image was well preserved, but that the self-face processing brain network was also actively engaged in processing his face after the injury.
After the transplant, the patient’s bias toward recognizing his pre-injury face persisted. His recognition of his post-transplant face gradually improved with time, however, so that by 20 months after the operation, its mental representation was comparable to that of his pre-injury face. This was reflected by a gradual increase in activity in the frontal lobe components of the self-face recognition network, which processes self-relevant information.
The researchers say that their results provide evidence for plasticity in the brain mechanisms underlying self-face recognition, but they point out that other face transplant patients could well respond differently. Emotional factors are likely to contribute hugely to how any individual responds to a face transplant and, indeed, preliminary studies with two additional patients revealed that each had unique responses to their tests.