Brain-zapping tech can improve memory by more than 50%
- When we encounter new information, neurons in a part of the brain called the hippocampus activate, sending electrical signals to other neurons in a particular pattern.
- A “memory prosthesis” uses electrodes to zap neurons in the hippocampus during memory formation. The idea is that this will help reinforce the pattern of electrical activity in the brain and improve the person’s ability to recall information later.
- The researchers observed memory improvements that range from 11% to 54%.
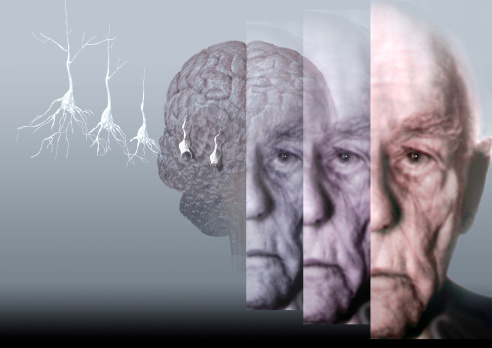
Brain injuries and diseases such as Alzheimer’s can disrupt our ability to form new memories. Depending on the severity of the memory loss, this can prevent a person from being able to work or live independently. It can also be incredibly traumatic.
“Loss of memory is probably the most tragic occurrence that can accompany disease or injury,” Robert Hampson, a neuroscientist at Wake Forest School of Medicine, said in 2018. “Memory is at the heart of who a person actually is … Without our memories, we lose our sense of self.”
Now, a new study suggests that a DARPA-funded “memory prosthesis,” which Hampson is helping to develop, could one day give people back their ability to make new memories — by shocking their brains in precisely the right way.
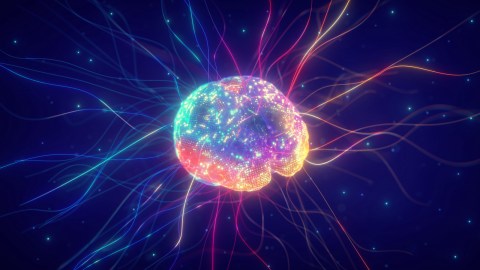
Making memories
When we encounter new information — say, learn a stranger’s name — neurons in a part of the brain called the hippocampus activate, sending electrical signals to other neurons. This pattern is then encoded in the brain, and when we need to recall the information later, the neurons fire in that same pattern.
If the hippocampus is damaged by disease or injury, the neurons can have trouble encoding the pattern in the brain — as a result, you may forget that new acquaintance’s name before the end of your first conversation.
“Loss of memory is probably the most tragic occurrence that can accompany disease or injury.”
ROBERT HAMPSON
The memory prosthesis being developed by researchers at Wake Forest and the University of Southern California (USC) uses electrodes to zap neurons in the hippocampus during memory formation.
The idea is that this will help reinforce the pattern of electrical activity in the brain and improve the person’s ability to recall information later — and based on recent human trials, it appears to work.
The science of brain zapping
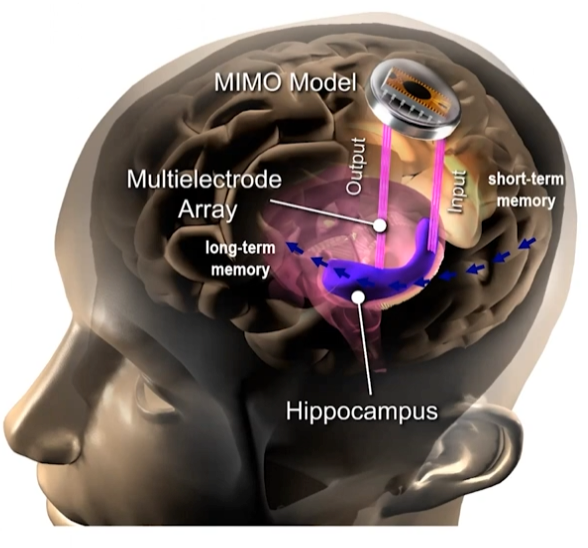
Through past research in both animals and humans, the researchers developed two versions of their memory prosthesis: a “memory decoding model” (MDM) and a “multi-input, multi-output” (MIMO) model.
The MDM model simply looks at the electrical activity in the hippocampus when a person correctly forms a memory and then comes up with an average pattern linked to successful memories. It then delivers that pattern back into the brain through electrodes when the person is trying to form a new memory.
The MIMO model is more advanced. It’s trained to analyze the electrical activity in the part of the hippocampus that receives new information (called the CA3 region), and then predicts the best pattern of electrical impulses in a different part (the CA1 region) for successful memory formation.
“The input to the model is live CA3 data recorded directly from a patient, and the model continually predicts what the CA1 output should be,” Sampson told Freethink. “We then use the output prediction as a pattern to stimulate CA1.”
For a recent study, the researchers tested their memory prosthesis in 24 people who already had electrodes implanted into their brains to help doctors study their epilepsy. Some of these people also had brain injuries and pre-existing memory impairment.
During the study, the participants completed simple memory tests while their brains’ electrical activity was recorded.
Each task started with showing an image on a screen. Up to 30 seconds later, the image was shown again, along with decoy images. The study volunteers then had to pick out the image they’d seen before.
Each person completed 100 to 150 of these tasks so that the researchers could personalize their MDM and MIMO models based on the individual’s brain activity.
“We’re seeing improvements that range from 11% to 54%.”
ROBERT HAMPSON
A few days later, the participants completed the memory tasks again. This time, some had their brains stimulated based on their personalized MDM or MIMO models, while some received random stimulation, and others received no stimulation at all.
Then, at least 30 minutes later, the participants completed “delayed recognition” tasks. These required them to look at a group of three images — one they’d been asked to remember previously, a previously seen decoy image, and a brand new image — and rank their familiarity with each.
Participants who received MDM or MIMO stimulation performed better on both kinds of tasks than those who received random or no stimulation. The more sophisticated MIMO model delivered the best results, on average, and the people with the worst memories at the start of the study saw the greatest improvements.
“We’re seeing improvements that range from 11% to 54%,” Hampson told MIT Technology Review.
Looking ahead
The new study confirms that precisely guided brain stimulation can improve a person’s ability to make new memories, but we’re still a long way away from a practical device that can help people with dementia or traumatic brain injuries regain lost memory function.
First, there are the hardware hurdles to overcome.
Hampson told Freethink a device to treat memory loss would need electrodes that can be permanently implanted — today’s electrodes develop scar tissue around them, which eventually causes them to fail.
We also need more advanced electrodes. The ones used during the study could only record from and stimulate 40-100 neurons, and USC researcher Dong Song told MIT Tech Review a device to treat memory disorders in the real world will need to be able to stimulate hundreds or thousands.
“We need to ensure that the approach works for everyone.”
ROBERT HAMPSON
More trials of the models are needed, too.
Testing them in people with epilepsy first made the most logistical sense because they were already undergoing the risky electrode implantation procedure, but that means we don’t know how well they’d work in people who don’t have epilepsy.
“We … need to pursue permission and volunteers to test the techniques in Alzheimer’s and possibly stroke patients as well to ensure that the approach works for everyone,” Hampson told Freethink.
Another challenge for the researchers is figuring out how to control the system to have the biggest impact — we don’t need to remember every new bit of information we encounter, and we can only store so much in our short-term memory.
“An implant has to either run continuously, or be smart enough to know when to turn itself on or off,” said Hampson.
The hippocampus isn’t the only part of the brain involved in memory formation, either, so if a person’s memory issues stem from damage elsewhere in the organ, they may need a different solution.
Still, with further development, it’s possible that this new memory prosthesis could not only help some people overcome memory problems, but give everyone a better memory one day — get the device implanted, and you’ll slash your chances of ever forgetting a name again.
This article was originally published by our sister site, Freethink. It is an installment of Future Explored, a weekly guide to world-changing technology. You can get stories like this one straight to your inbox every Thursday morning by subscribing here.