Scientists convert kidney to universal type O blood

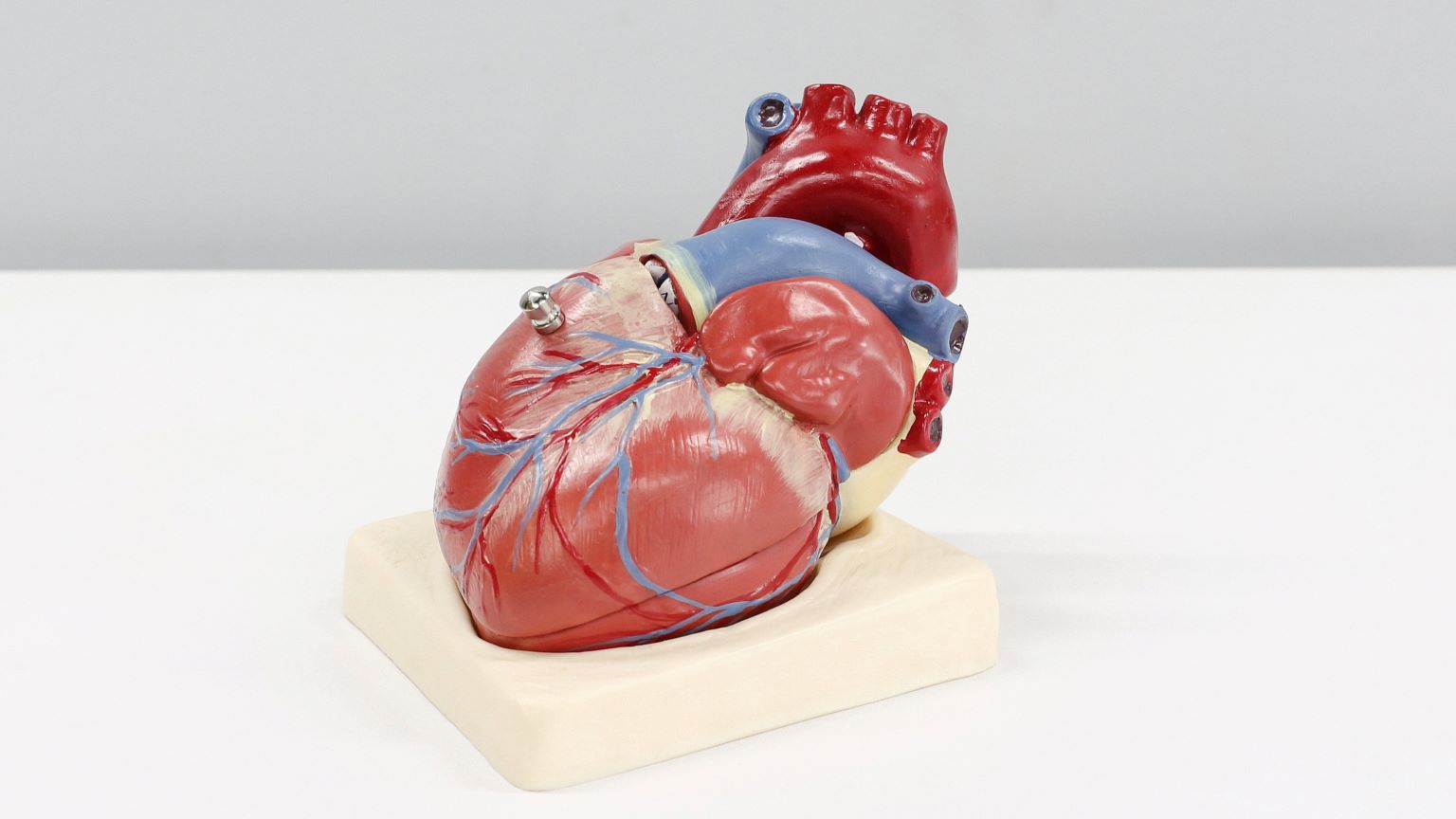
- To receive a transplant, a kidney and its recipient must have matching blood types.
- Type O is the “universal” blood type, which means that people of any blood type — A, B, AB, or O — can receive O blood.
- Organs still need to be tissue-matched, but by converting a kidney to type O, more will be available for transplant.
For transplant candidates from ethnic minorities, the wait for an acceptable organ can be even more grueling than for others.
Type B blood is more common in minority communities, making type A organs incompatible.
But a breakthrough by Cambridge researchers could dramatically change the rules for transplant compatibility.
In a recent experiment, they changed a kidney’s blood type from A to the universal type O — making it theoretically available for any patient, including those with type B blood.
Type B blood is more common in minority communities, making type A organs incompatible.
“We know that people from minority ethnic groups can wait much longer for a transplant as they are less likely to be a blood-type match with the organs available,” Aisling McMahon, the executive director of research at charity Kidney Research UK, which funded the work, said.
“This research offers a glimmer of hope to over 1,000 people from minority ethnic groups who are waiting for a kidney.”
“I feel sad at the thought of waiting so long”: Ayesha was diagnosed with stage 3 kidney disease in 1998, and lived with the disease until the pandemic, when her kidneys began to deteriorate quickly.
Put on the transplant list, she was told she may need to wait twice or even three times as long as a white patient.
“They explained that because of my ethnicity my wait for a deceased donor will be longer than for a white person,” she told Cambridge.
In the UK’s Muslim commnuity, kidney disease is common but not talked about, says Ayesha, who recently began volunteering for Kidney Research UK.
“I feel sad at the thought of waiting so long for a transplant, I understand a transplant isn’t a cure, but it would make my body a lot stronger and give me a second chance at a healthy life.”
The Cambridge work, led by professor of transplant surgeon Mike Nicholson and PhD student Serena MacMillan, may help patients like Ayesha become eligible for kidneys much faster, if it is proven safe and effective in the clinic.
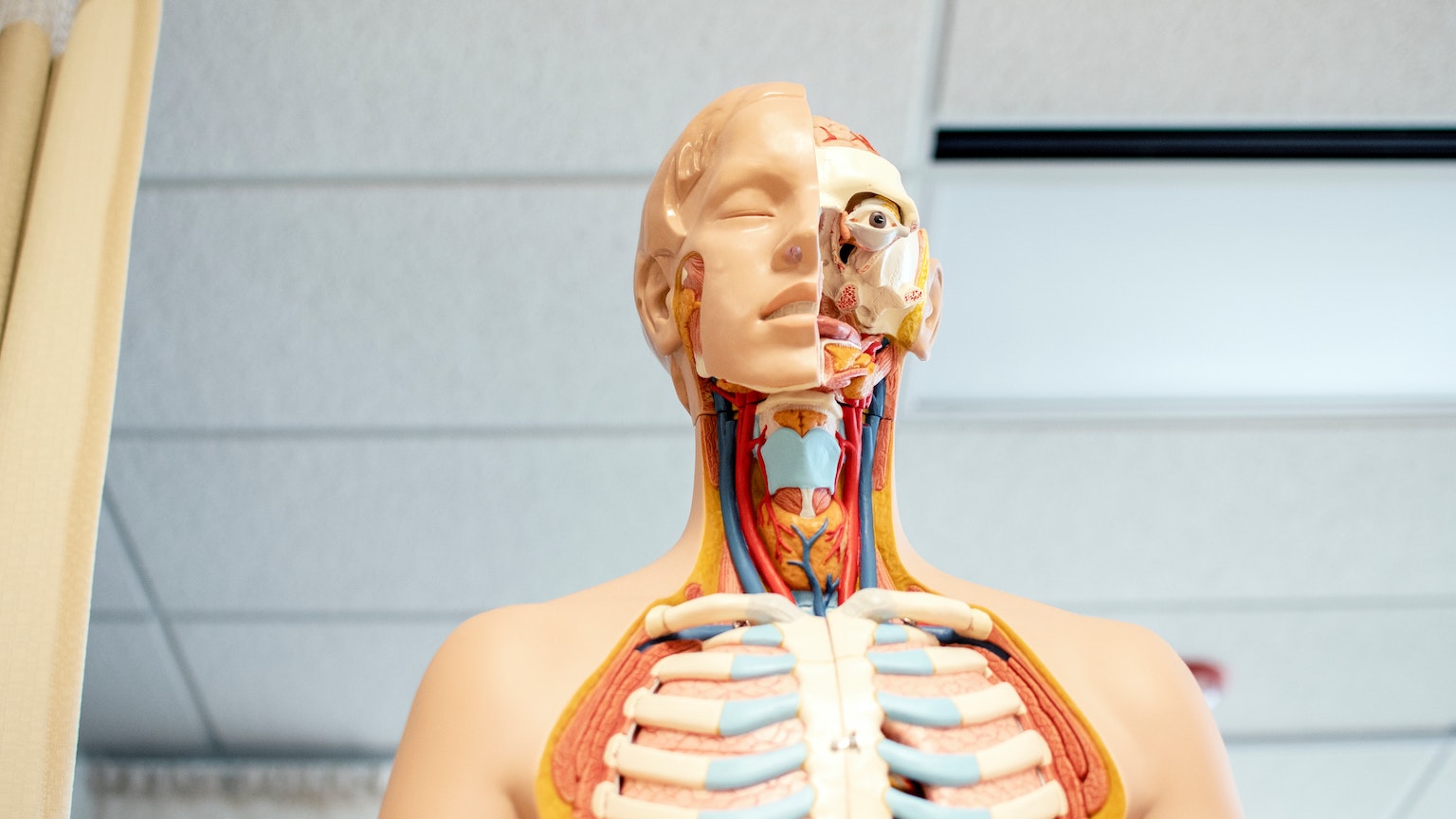
To your body, transplanted organs need to be attacked like viruses or tumors, and non-matching blood types exacerbate the issue.
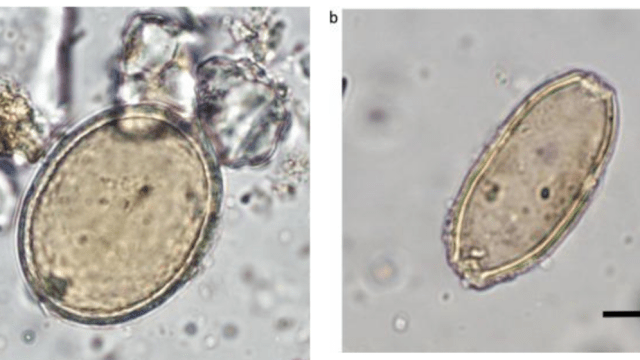
Changing types: To your body, a transplanted organ is something alien that needs to be attacked — just like bacteria, viruses, tumors, and parasites.
Non-matching blood types exacerbate this issue.
“One of the biggest restrictions to who a donated kidney can be transplanted to is the fact that you have to be blood group compatible,” Nicholson said.
“The reason for this is that you have antigens and markers on your cells that can be either A or B. Your body naturally produces antibodies against the ones you don’t have.”
To change a kidney to type O — which can be universally accepted — the team took aim at those antigens.
Using a machine called a normothermic perfusion machine, they flushed three deceased donor kidneys with blood containing an enzyme that works like a pair of “molecular scissors,” slicing out those A or B antigen blood markers.
With those markers stripped away, the kidneys became type O in just a few hours.
“Our confidence was really boosted after we applied the enzyme to a piece of human kidney tissue and saw very quickly that the antigens were removed,” MacMillan said, referring to an earlier experiment.
“After this, we knew that the process is feasible, and we just had to scale up the project to apply the enzyme to full-size human kidneys.”
The team’s research is scheduled to be published in coming months in the British Journal of Surgery. Similar work has previously been performed in lungs.
The great hurdle: In my previous reporting on the field, I’ve been told that rejection of organs is, essentially, the only limit to transplant surgery, according to top-flight transplant surgeons at Massachusetts General, Johns Hopkins, and South Africa’s Stellenbosch University.
The immune system’s attack on alien tissue can be defeated in various ways, including the standard approach: lifetime immunosuppression. While this often works, it also leaves the body highly vulnerable to infection — and still does not guarantee the organ won’t be rejected eventually.
The team flushed the kidneys with special enzymes to convert them to blood type O — the universal donor.
Researchers are racing to find other ways to prevent organ rejection, including transplanting bone marrow tissue at the same time, to fool the body into thinking the organ is natural — known as mixed chimerism — and, more rarely, essentially transplanting a whole new immune system via stem cells.
The Cambridge researchers hope their technique may join that growing toolbox, although it is important to note the research is still ongoing.
Using the same machine they used to change the kidneys’ blood type, the team will now test how the freshly christened type O kidneys react to blood of different types, a simulation of what will happen when introduced to a patient.
From there, they will begin figuring out how to test the technique with transplant patients.
“The research will offer so much hope to minority groups still waiting for a transplant and could help to save many lives,” Ayesha said.
This article was originally published by our sister site, Freethink.