New obesity drug cut weight by 58 pounds in a trial, the most effective yet

- Eli Lilly’s new obesity treatment, retatrutide, caused patients who received the highest dose to lose an average of 58 lbs (26.3 kg) after a 48-week treatment course.
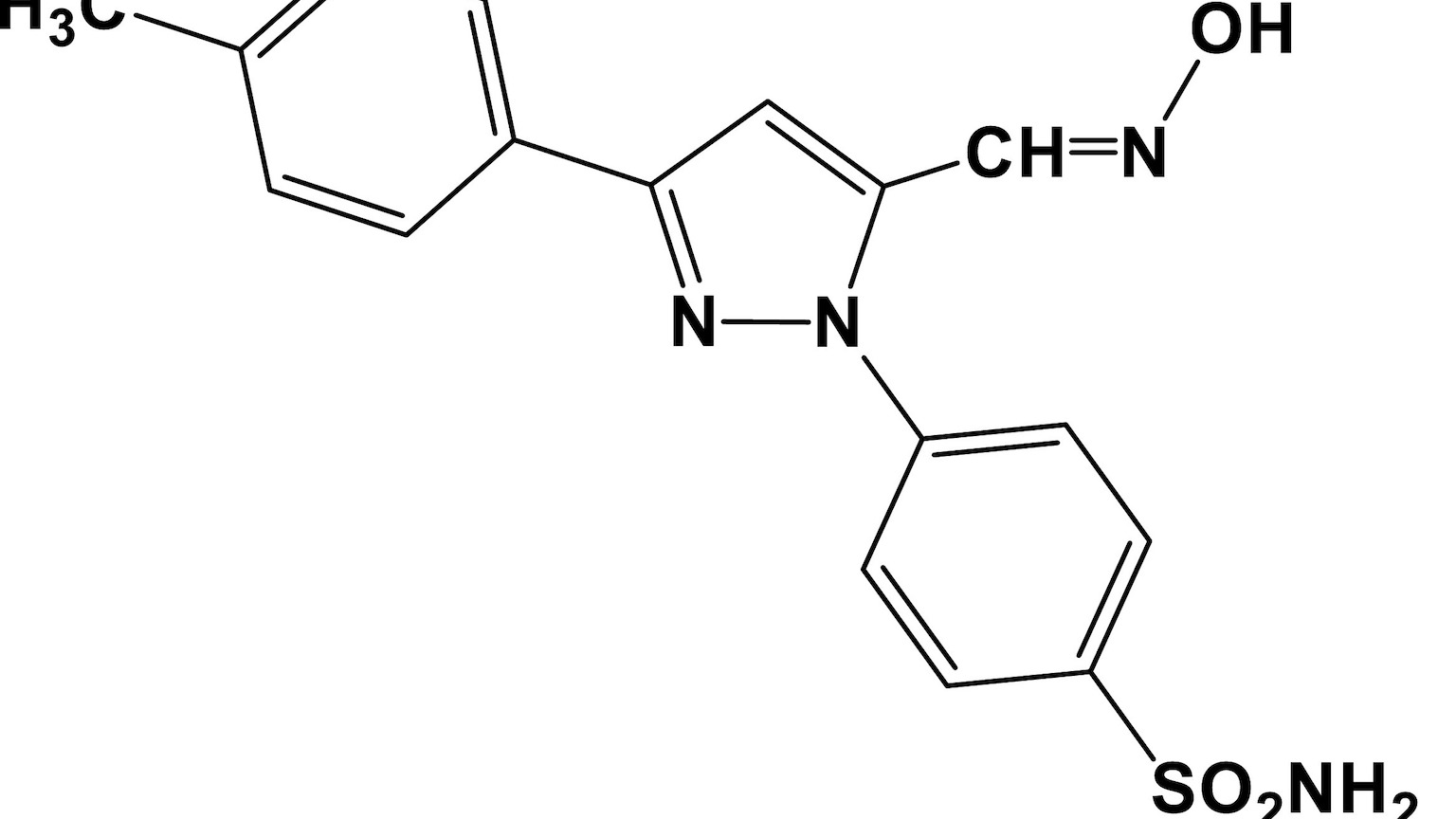
- The drug, which is part of the glucagon-like peptide-1 agonists (GLP-1) class, is designed to boost insulin, regulate blood sugar, slow down stomach emptying, and decrease appetite.
- The trial also found that retatrutide significantly reduced fat in the liver, suggesting it could treat non-alcoholic fatty liver disease.
Indianapolis-based Eli Lilly has published the results of a clinical trial of its new obesity treatment. The phase 2 trial, published in the New England Journal of Medicine, showed patients losing 58 lbs (26.3 kg) on average, at the end of a 48-week treatment course.
The results catapult the drug, an injectable called retatrutide, into a rapidly-crowding class of new weight loss drugs, whose dramatic results are driving social media fervor and pharmacy shortages.
Eli Lilly’s new obesity treatment showed positive results in a phase 2 trial.
Best known is semaglutide (sold under brand names Ozempic/Wegovy), an injectable drug made by Novo Nordisk; the Danish pharma giant also made waves with recent positive data for a pill version of the drug. Pfizer is looking to enter the oral obesity treatment race, as well (while scratching one drug candidate over concerns about potential liver damage). And Lilly already has one impressive candidate, tirzepatide (sold as Mounjaro for diabetes treatment), whose weight loss effect is at least as large as semaglutide.
“Obesity is a treatable chronic disease with a complex underlying biology,” Ania Jastreboff, director of the Yale Obesity Research Center, said in a statement released by Lilly. “We are now in the midst of a rapidly expanding therapeutic landscape of potential highly effective treatment options for individuals with obesity.”
What are GLP-1 agonists? The drugs are all part of the same class: glucagon-like peptide-1 agonists (GLP-1 for short). Already used for years to treat diabetes, GLP-1 agonists are designed to copy their namesake hormone, which boosts insulin, regulates blood sugar, slows down the emptying of the stomach — and, most notably, decreases appetite.
This last effect appears to drive a lot of weight loss. In clinical trials, semaglutide has reduced weight by around 15%, in both injectable and pill forms. Tirzepatide, which also targets another receptor besides GLP-1, cut weight by up to 20% at its highest dose, in a recent trial. The 24% decline for the highest dose of retatrutide, which hits three receptors, is the most yet seen for this class.
Lilly’s nickname for retatrutide is “triple g,” for its three-pronged mechanism. As you may have guessed, one of those Gs is for GLP-1. The drug also targets a second obesity-linked hormone, GIP, as well the body’s receptors for glucagon itself.
“We believe that combining glucagon receptor agonism with GIP and GLP-1 receptor agonism may be one of the reasons retatrutide showed this level of weight reduction,” Lilly chief scientific and medical officer Dan Skovronsky said.
Patients on all doses showed a mean loss of 41.2 lbs, with patients on the highest dose losing on average 57.8 lbs — and still dropping.
The trial: The phase 2 study was a randomized, placebo-controlled, double-blind study evaluating the efficacy, safety, and tolerability of various doses of retatrutide. It enrolled 338 patients with obesity and weight-related conditions, except type 2 diabetes.
Volunteers were randomized into groups that received varying doses of retatrutide at multiple escalation schedules — topping out at 4mg, 8mg, or 12mg — or a placebo delivered via injection once weekly for 48 weeks.
The study’s primary endpoint was the amount of weight a patient lost compared to their baseline at the 24 week mark. At the 24 week mark, patients on all doses showed a mean loss of 41.2 lbs, with patients on the highest dose losing on average 57.8 lbs — and still dropping.
“Given that participants had not yet reached a weight plateau at the time the study ended, it appears that full weight reduction efficacy was not yet attained,” Jastreboff said. “Longer duration phase 3 trials will enable comprehensive evaluation of efficacy and tolerability of this potential pharmacotherapeutic for the treatment of obesity.”
As FiercePharma points out, the results “blow out of the water” the data from the currently approved options, Novo’s Ozempic and Lilly’s Mounjaro.
The caveats: These drugs’ success when it comes to dropping pounds is impressive, but it does come with some caveats. Common side effects are gastrointestinal upset, including diarrhea, nausea, and vomiting, but they tended to be tolerable to people in clinical trials. More serious concerns include elevated heart rate, and the less common but more serious risks of kidney damage.
A recent concern raised by anecdotal reports is that patients, in addition to losing fat, may be disproportionately losing lean body mass (e.g. muscle), as well. The jury’s still out on this one, but people losing weight almost always lose lean mass as well as fat. Studies have found these drugs’ effects on body composition fall generally in line with other weight loss methods, including diet and bariatric surgeries.
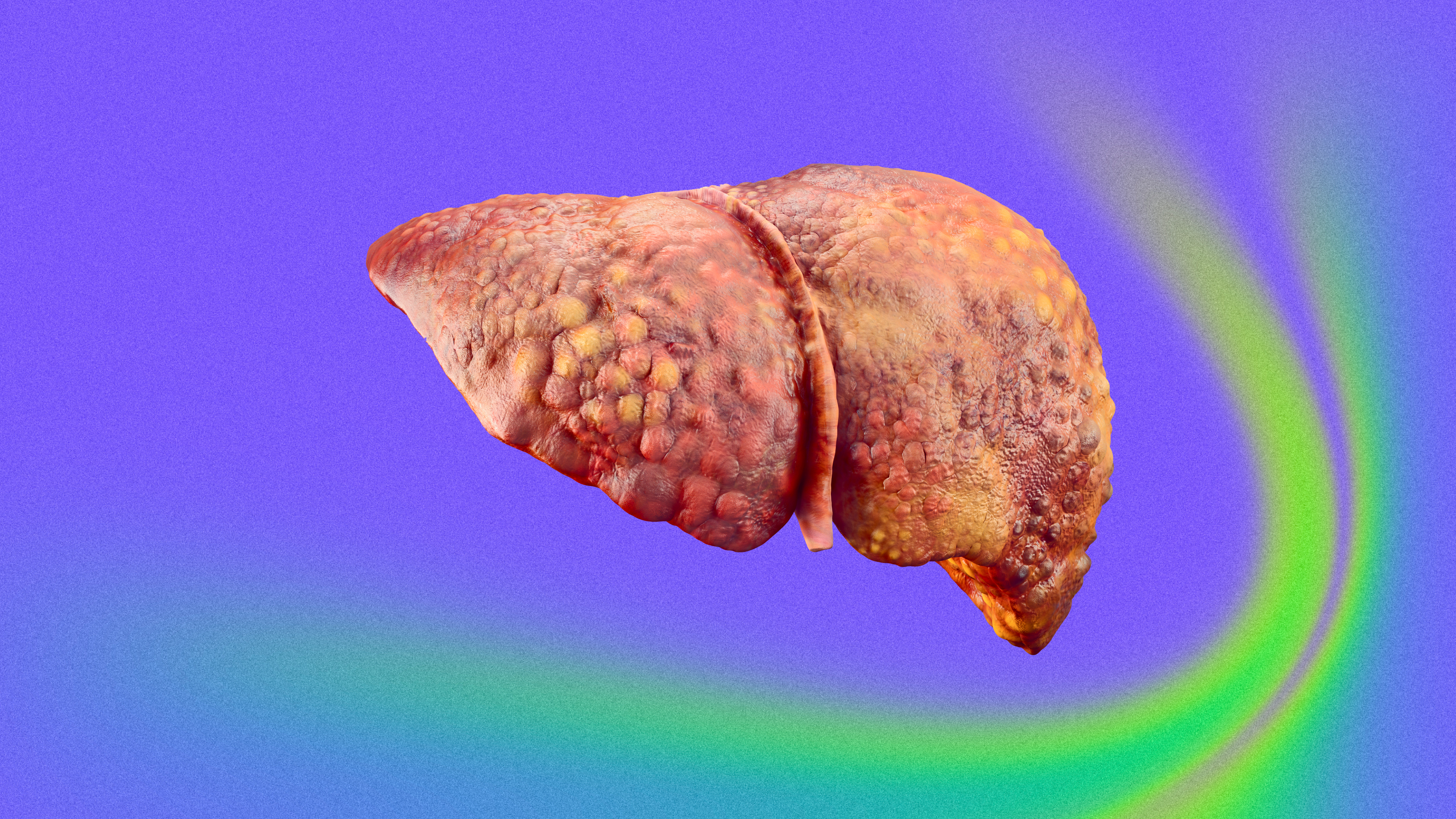
The recent Lilly trial also found that retatrutide reduced fat in the liver, suggesting it could treat non-alcoholic fatty liver disease (NAFLD).
All of these concerns must be weighed against the constellation of health concerns tied to obesity itself, including heart disease, stroke, type 2 diabetes, hypertension, depression, and some forms of cancer.
The recent Lilly trial also found that retatrutide massively reduced fat in the liver, suggesting it could treat non-alcoholic fatty liver disease (NAFLD), an increasingly common cause of liver damage and failure in the United States.
Lilly is running a longer and larger phase 3 trial of the drug, Reuters reported, which will provide more data on its efficacy and safety profile.
This article was originally published by our sister site, Freethink.