CRISPR cure for HIV now tested in 3 patients
- Antiretroviral therapy is incredibly effective at controlling HIV, but it does not cure patients of the virus.
- Excision BioTherapeutics is using the gene-editing technology CRISPR to cure HIV.
- The hope is that a cure would free patients from a lifetime of antiretroviral therapy.
California-based biotech company Excision BioTherapeutics has shared data from the first human clinical trial of a CRISPR cure for HIV — and it’s both encouraging and frustratingly light on details.
The challenge: HIV is no longer the death sentence it once was, thanks largely to antiretroviral therapy (ART), daily medications that can decrease the amount of the virus in a person’s blood to levels that are undetectable and untransmittable.
ART doesn’t cure HIV, though — it just forces the virus to enter a dormant state, hiding its DNA in a person’s immune cells. If the person with HIV stops taking their ART, the virus can become active again, potentially leading to new symptoms and even death.
EBT-101 instructs a CRISPR system to hunt down the HIV hiding in a person’s cells.
CRISPR cure for HIV: Excision BioTherapeutics is one of several groups exploring the use of the gene-editing technology CRISPR to outright cure HIV, freeing people from a lifetime of ART.
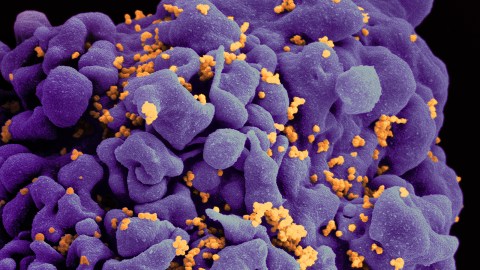
Their treatment, EBT-101, instructs a CRISPR system to hunt down the HIV hiding in a person’s cells and make three cuts to the HIV genome. Those cuts are designed to break the genetic recipe for the virus and eliminate any possibility of it reemerging.
What’s new? After promising studies in mice and non-human primates with SIV — the monkey version of HIV — the Excision team launched a clinical trial of its CRISPR cure for HIV in 2022.
On October 25, 2023, they shared the first data from the trial at the European Society for Gene & Cell Therapy’s annual meeting in Brussels, Belgium — but missing from the announcement was any data about whether the therapy worked.
None of the patients experienced serious adverse effects from the CRISPR therapy.
What we know: During the presentation, the Excision team announced that it had administered a single IV infusion of EBT-101 to three people with HIV. All three had undetectable levels of HIV prior to starting the study, thanks to ART.
None of the patients experienced serious adverse effects from the CRISPR therapy, and the four mild adverse effects observed all resolved on their own. Four weeks after treatment, EBT-101 could be found in the blood of all three participants.
The missing link: While the primary purpose of the trial is to test the safety and tolerability of the CRISPR therapy, the researchers also planned to have “all eligible participants” stop taking ART 12 weeks after receiving EBT-101 to see if their HIV rebounded. (The therapy would be restarted again if it did reemerge.)
It’s not clear what makes a trial participant eligible, but at least one of the patients received the CRISPR therapy more than a year ago. If they stopped taking their ART, Excision isn’t ready to share whether the treatment prevented or delayed their HIV from returning.
Excision promises to present more trial data in 2024.
Looking ahead: In the next phase, Excision plans to administer a larger dose of EBT-101 to six more trial participants in the fourth quarter of 2023. This dose escalation was planned from the start of the study, so it doesn’t indicate whether the smaller dose did or didn’t work.
As for when we’ll find out whether a CRISPR cure for HIV is within our grasp, Excision promises to present more trial data in 2024.
Whether or not any of these patients were cured, larger trials will be needed to get more definitive answers about the treatment’s safety and efficacy. But EBT-101 is not the only lead in the hunt for a universal HIV cure — we also have stem cell transplants, medications, and other CRISPR therapies showing promise against the elusive virus.
This article was originally published by our sister site, Freethink.