Can synthetic biology protect us from coronavirus? And the next one?

(Photo: U.S. Department of State)
- The first coronavirus vaccines will enter Phase 2 testing soon but won’t be ready for another 18 months.
- Synthetic biology may offer a “universal coronavirus vaccine” that can be quickly modified to combat future mutated forms.
- Despite promising lab tests, synthetic vaccines remain speculative; we’ll need to live with COVID-19 during the interim.
The world was not prepared for coronavirus. Despite the clarion calls that were the SARS and MERS outbreaks and early warnings from doctors, governments had neither the policies nor equipment in place to impede COVID-19’s spread from a Chinese animal market.
The United States’ strategy was to impose a medical bubble of travel restrictions and mandatory quarantines. “We have contained this. I won’t say airtight but pretty close to airtight,” White House National Economic Council Director Larry Kudlow said last month—despite contrary warnings from Centers for Disease Control and Prevention (CDC) officials.
At that time, there were a handful of known cases. As of March 11, more than 1,000 people across 38 states have tested positive for the disease.
For many hope lies in the development of a vaccine, but while the first vaccines should enter Phase 2 testing by summer, that leaves an efficacy-tested product months away. Anthony Fauci, head of the National Institute of Allergy and Infectious Disease, estimates the first vaccines won’t be ready for “a year to a year-and-a-half.”
As companies hurry to test potential vaccines, the National Institute of Health (NIH) is hoping new bio-engineering techniques to help us restrain coronavirus—and its next mutation, too.
Engineering a solution
As reported by Sharon Begley in STAT, NIH is looking toward synthetic biology for the next advancement in vaccination development. This research is funded, in part, by the Bill and Melinda Gates Foundation’s $100 million commitment to strengthening global “detection, isolation, and treatment efforts” directed at COVID-19.
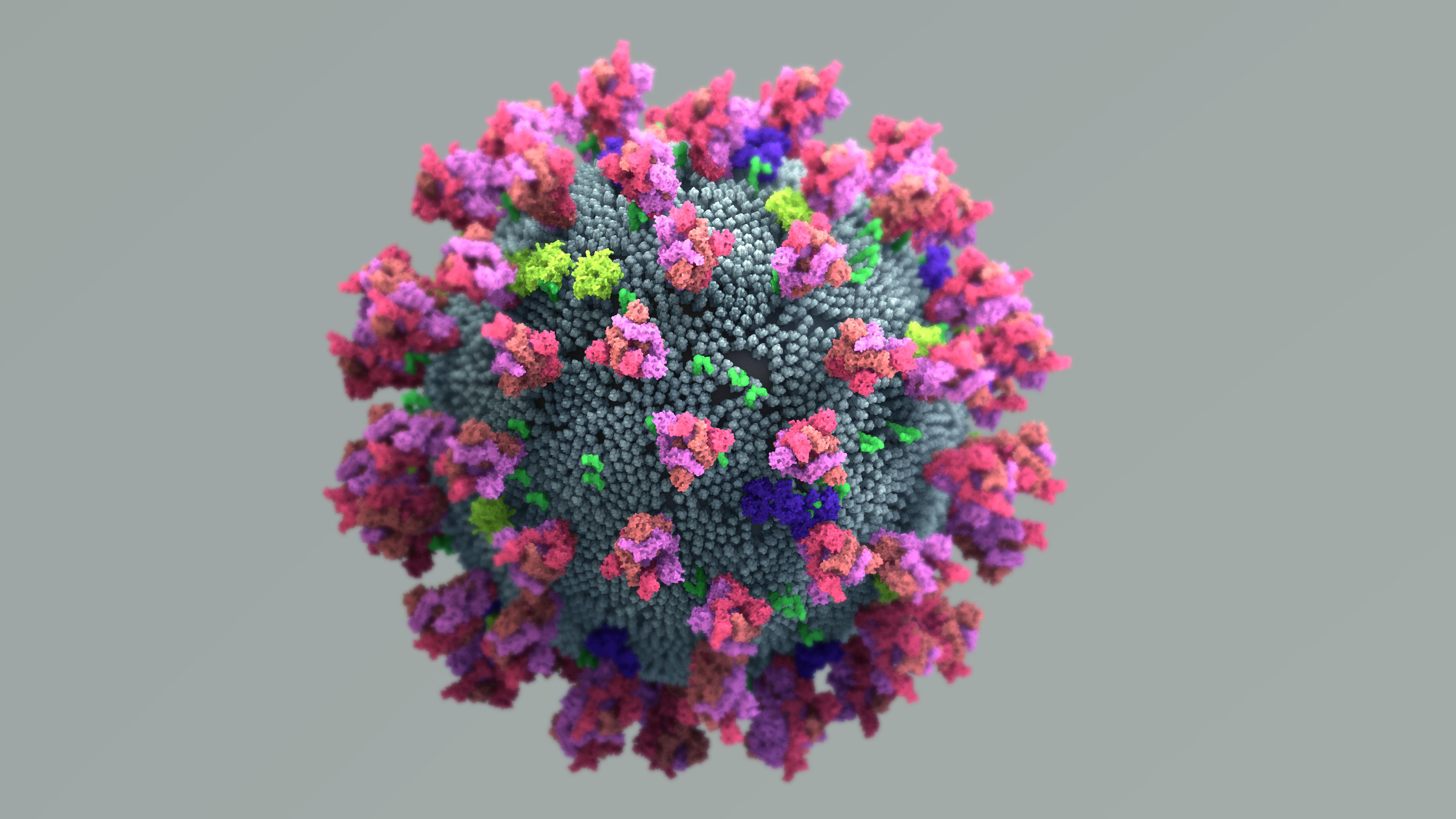
In synthetic biology, scientists re-engineer organisms to sport new abilities or biological purposes. They do this by stitching together strands of DNA and inserting them into an organism’s genome. This artisanal DNA can come from other organisms or be a completely original strand.
Scientists begin the process by engineering nanoparticles out of proteins. Using a computational algorithm, they experiment with a million variants to discover the optimal structure. This structure not only allows the nanoparticle to house the viral antigens, but arranges those antigens for maximal arousal of the body’s immune response.
After lab-crafting DNA to code for the nanoparticle, the scientists place it in E. coli bacteria. Once the bacteria begin manufacturing the desired protein, it is extracted, purified, and studded with viral antigens.
“If tests in lab animals of the first such nanoparticle vaccine are any indication, it should be more potent than either old-fashioned viral vaccines like those for influenza or the viral antigens on their own (without the nanoparticle),” Begley writes.
According to Lynda Stuart, immunologist and physician who directs the Gates Foundation’s vaccine research, synbio vaccines may have advantages beyond potency. The increased immune response could eliminate the need for adjuvants (additives used to boost said response). They could reduce the need for refrigeration, making deployment to poor countries easier. And they could be designed to house antigens from several viruses, making one vaccine capable of fighting multiple diseases.
The ability to take past viral designs and quickly retrofit them to new, mutated forms of a virus could also reduce the development time for new, necessary vaccines.
“We may need an approach that can get you millions and even billions of doses,” Stuart told STAT.
Synbio vaccines are still in the preliminary phases, and more traditional vaccines won’t be available for months. During the interim, the virus will continue to spread, and its novelty means we’ll need to encounter it before our bodies can build immunity. Many will become sick, but few will develop serious illness.
As Nancy Messonnier, director for the National Center for Immunization and Respiratory Diseases, notes in the video above, the disease affects older adults most seriously. The greatest risk is faced by people over the age of 80 and those with underlying health conditions.
Without a vaccine to curb its spread, it will be up to us to do what we can to maintain our health and prevent spreading the disease.
Wash your hands. Americans are awful when it comes to hand hygiene, but it’s one of the best ways to prevent the spread of disease. Wet your hands with warm water, lather them with soap, and scrub them all over for 20 seconds. Rinse your hands, and finish with a paper towel or air dry.
Hand sanitizers can work, but they have to be rubbed in for 20 seconds and contain at least 60 percent alcohol. You should also sanitize frequent-contact surfaces like smartphone screens.
Stay home if you are sick. It’s good advice in general as your fellow students and coworkers don’t need you to share your lung grimes. But it’s especially important to do so if you have coronavirus symptoms. If your symptoms become serious, contact a doctor for instructions and the next steps.
Limit potential exposure. If you are at higher risk, you’ll want to avoid crowds as much as possible, especially in poorly ventilated places. You should also avoid non-essential plane travel.
Have supplies on hand. You don’t need a doomsday prepper’s supply, but make sure you have a two-week supply of the essentials on-hand in case you get sick and have to stay in. If you have an underlining medical condition, ensure you have enough medication on hand.
Face masks. If you are healthy, you likely do not need to wear a face mask for protection. The CDC advises face mask use for people who have COVID-19, are showing symptoms, and do so under the recommendation of a healthcare professional as it may prevent them from spreading the disease to others. Wearing a face mask needlessly limits the necessary supply available to health and care providers.
Stay informed. Visit the CDC’s coronavirus website for situation updates and information on the virus. Don’t rely on hearsay or social media to inform you about local conditions. Monitor your state and local health department websites instead for accurate, reliable information.