Defining mental illnesses as precisely as bodily disorders will require more advanced neuroscience, but also a deeper understanding of insanity’s cultural context.
Question: What contemporary psychiatric diagnoses do you believe are based on faddish social thinking?
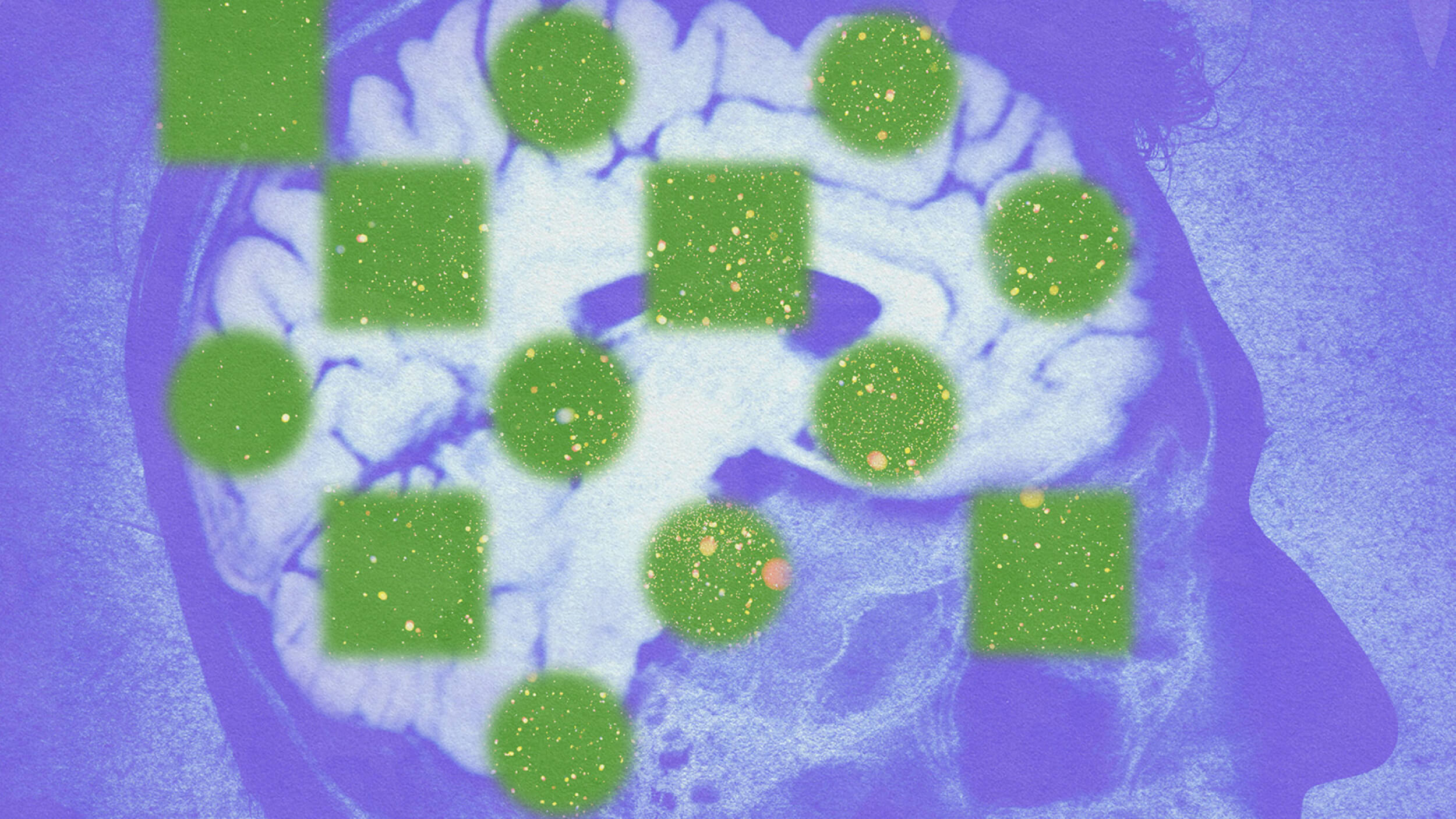
rnJonathan Metzl: Well you know, again, I’m a practicing psychiatrist and I think that I really believe in the advances of psychiatry. Our diagnoses are more precise. They get more precise with every volume of the Diagnostic Manual. Our treatments slowly get better over time and I’m not averse to saying that there are biological basis to mental illness. I’m part of a department that does a lot of fantastic research in brain imaging, scans, other kinds of genetic research that really looks at mental illness seemingly below the level of culture, context, race, ethnicity, at the level of brain structures that are seemingly the same in all people, and at the same time I feel like there is a false divide, almost like you have to vote, is an illness biological or is it social or socially constructed, and I don’t like that divide very much because I think that all definitions of illness and maybe particularly all definitions of psychiatric illness are always both. It doesn’t have to be one or the other. Mental illness is a real thing. It has real material consequences for people who suffer from it and at the time even the most biological finding reflects social context in very important ways, and so I think psychiatry is better off looking both at biology and at social context and really trying to think of the relationship between these and I think doctors and patients are better off that way. We certainly know that depression is an illness. All you have to do is watch an antidepressant advertisement on television right now and think about why might it be that a person might see an ad like that. What are the forces that are leading them to go in and ask a doctor? In part it might be that that ad speaks to some symptoms they’re having that are chemical symptoms, but many of these ads play off of familiar cultural stereotypes about gender or parenting or social class, other kinds of things and so I think doctors need to be aware of both that. Depression as one example is an illness that has a chemical basis, but also is deeply embedded in cultural norms about gender, social class, race, so that would be one example. There is great work that has been done now on bipolar disorder by Emily Martin here at NYU and looking at the kind of cultural basis of bipolar disorder. Obsessive-compulsive disorder after the show Monk, for instance, is something that there is a lot of popular conversation about and so I think again it’s true for all illness, but it’s certainly true for psychiatric illness that these illnesses often reflect cultural norms in addition to biological realities, and really we have to be fluent in both.
rnQuestion: Will mental disorders ever be defined as precisely and universally as bodily disorders?
rnJonathan Metzl: Right, well again, I think that we’re making a mistake if we don’t see that there is a cultural basis to many illnesses, not just psychiatric ones. Breast cancer would be one prevalent example right now, different kind of cultures surrounding it. If you don’t understand the cultural meaning of an illness like that you’re going to miss the boat even if you’re a great scientist. So I don’t think it’s the case that it’s just psychiatric disorders, but we know from history that when we get the ultimate, you know, cure for a particular illness or nail it down it stops being a psychiatric illness and then it’s taken up by internal medicine or, you know, we know, oh, it was just and iron imbalance or it was a vitamin deficiency or something like that, but in a way it’s taken from psychiatry and taken to medicine. But I think that you know if you look at diagnostic rates and treatment rates in psychiatric disorders it’s - even with all the controversy about SSRIs right now the improvement rates are reasonably good compared to other medical specialties, and so I think it’s always going to be a negotiation about what is the best way to understand psychiatric illness, but of course the flip side of that is that there is this aura of it’s something we don’t know in a certain kind of way, and so psychiatry is always kind of fighting against that, and probably that’s why we had a move toward saying things are solely biological in a certain kind of way is to, you know, rightly move toward a more scientific basis.
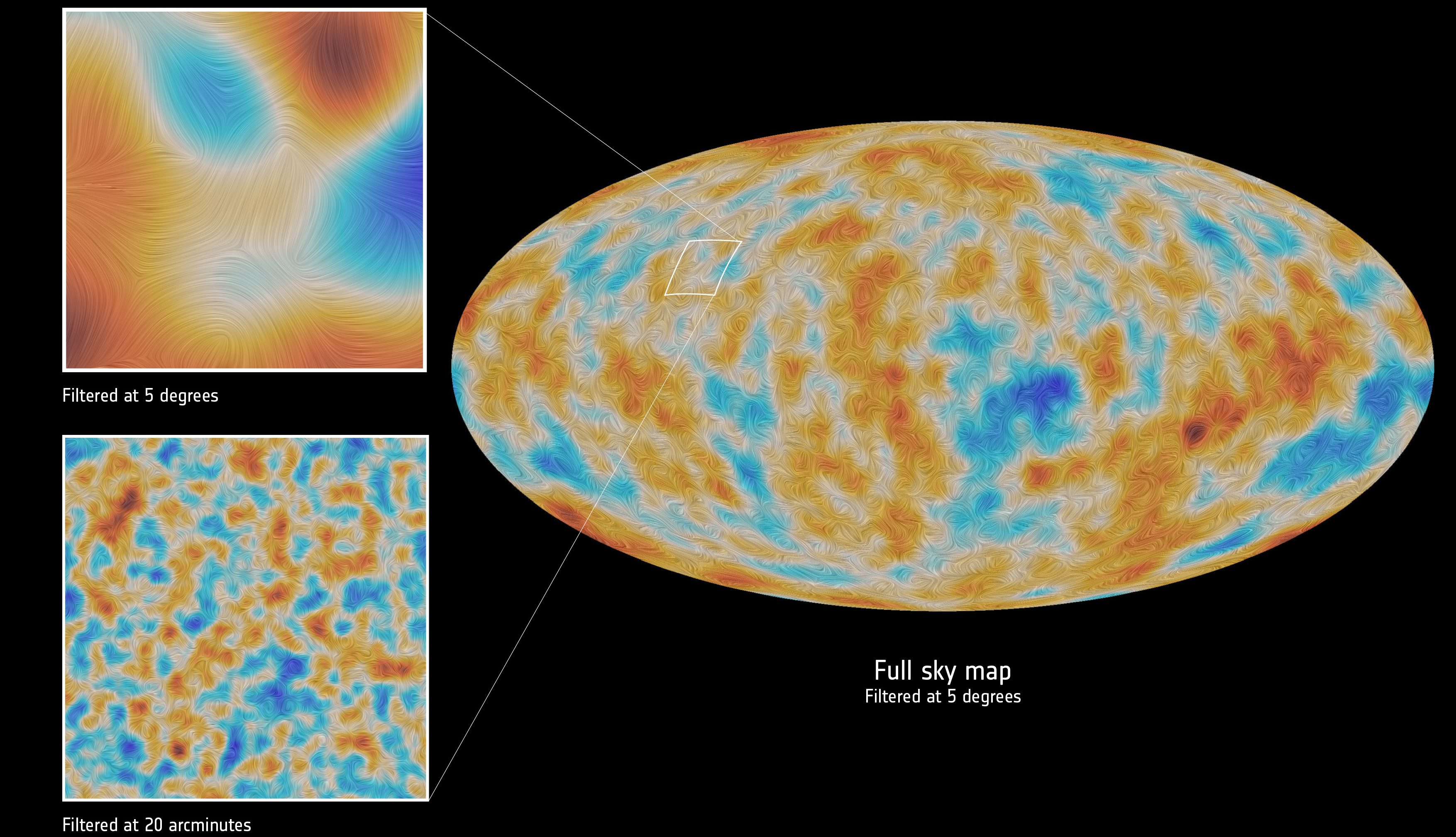
rnQuestion: How will more advanced neuroscience and neurological treatments change psychiatry?
rnJonathan Metzl: Terrific. Well I mean it’s, there are really exciting things happening in genetic and neurobiology right now, and really looking at the ways in which different not just illnesses, but social conditions and social pressures can actually lead to actual brain changes. You know there was a lot of promise in the development of pharmaceuticals, particularly with the advent of a newer generation of antipsychotics and antidepressants, and we know from history that there is a kind of natural trajectory of the way that these medications come out and are accepted. So initially we say these are cures for everything under the sun and there is this dramatic rise and then we say wait a minute, these don’t work for anything, which I think is happening with the SSRI antidepressants right now, and then we kind of figure out a moderated use of, well, they’re good for some conditions and not for others. And so again as I say, I think that there is a give and take that is part of the process and part of it is based in science, but I also think, you know, the 1990s were often called the decade of the brain in psychiatry where we didn’t need to worry about Freud or about gender or psychoanalysis, context. All these things were in certain ways kind of pitched out the window because we were going to get the answer to everything from brain scans. And I think psychiatry itself has come to, in a way like medications, a more moderated understanding of the brain itself is very important, but you don’t really know anything about the brain unless you know about social context, expectations, stigmas, other kinds of things, and so hopefully these findings will continue to be understood in social context.
Recorded on January 29, 2010
Interviewed by Austin Allen