New research by Xavier Castellanos suggests that the key to diagnosing mental illness might have to do with how the brain communicates with itself during sleep.
Question: What is the future of dealing of diagnosing and treating mental illness?
Harold Koplewicz: I think one of the most exciting phenomena has been elucidated and really brought to the forefront by Dr. Xavier Castellanos, a child and adolescent psychiatrist who, years before, a decade ago, was telling us that the real action in the brain is while the brain's at rest, not while the brain is doing stuff. And so you have to understand that when we were trying to find... we’re looking for the biomarker, we’re looking for the equivalent of a blood test. If you come into a doctor’s office and you are coughing and you have a chest cold and the cold makes you feel terrible, we can do a blood test and tell you whether or not it’s a virus or if it’s bacterial. If it’s bacterial, we give you antibiotics. If it’s a virus, we just wait for the virus to die. You will live longer than the virus, so we give you stuff to make you feel better, whether it’s Tylenol or it’s aspirin, it’s plenty of fluids. But there’s no medicine to make it go away.
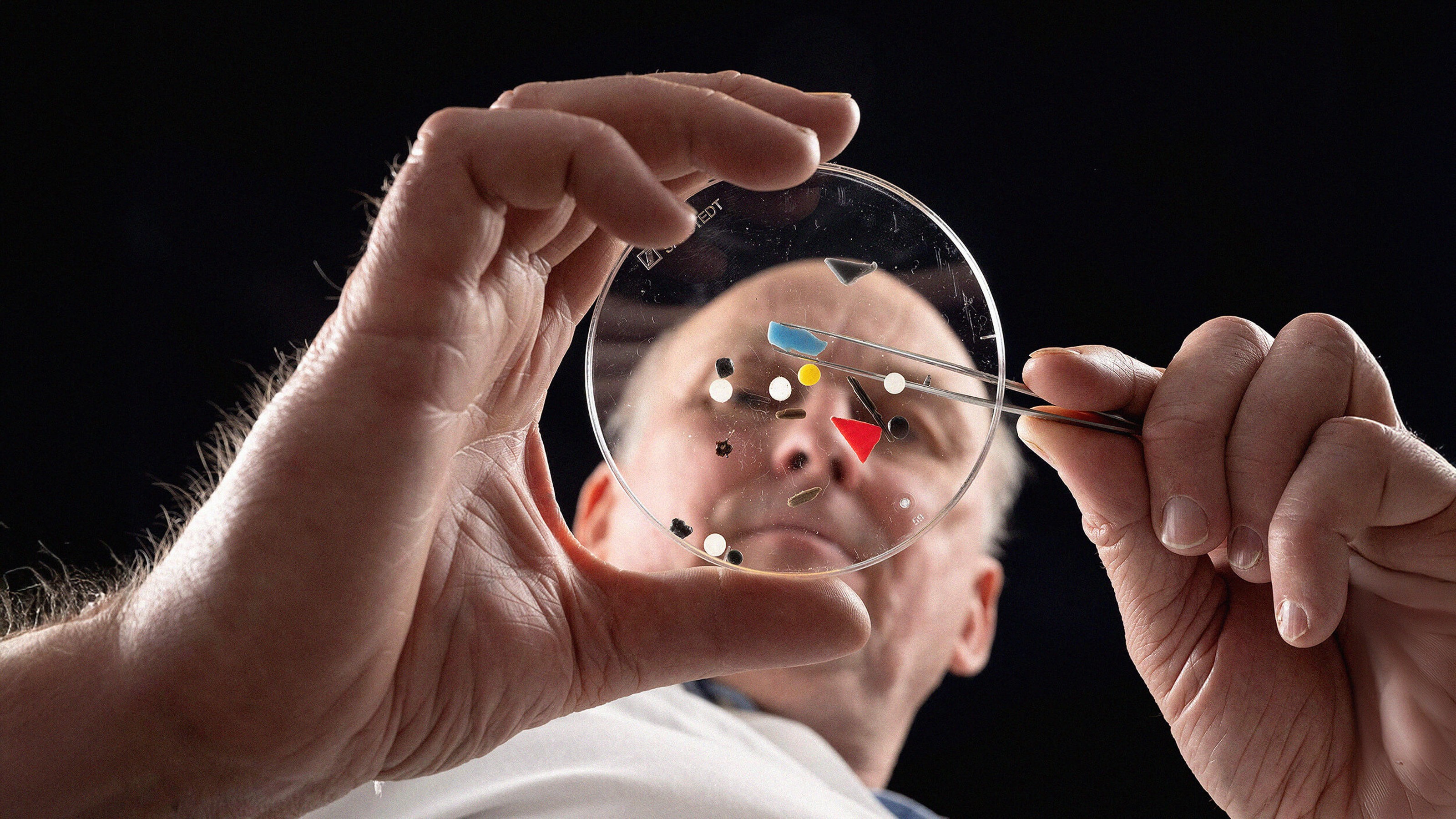
We don’t have that in psychiatry. That’s the Holy Grail: "What’s the biomarker?" And so when the MRI came in—or the CAT scan first—but the MRI became the new way to look at the brain, these neuroimaging tools. And so first came the structural MRI. To look at how does the brain... how is it built? And is it built differently in people who have a certain psychiatric illness versus a normal, versus someone with a different kind of psychiatric illness. And while that gave us some hints as group differences, it wasn’t as specific as the functional MRI, which would actually take a look at your brain and see how it works.
Now, originally we would put kids, or adults, into this machine and have them do a task so that if you had a social anxiety disorder and so seeing faces that you knew versus faces that you didn’t know should activate different parts of your brain. And it was very hard to find a difference when you showed these tasks or made these tasks.
And so what happened was, Castellanos said, this is kind of like the post office. When the post office is closed, there’s a lot of action going on there. That’s when people are talking to each other, they’re moving bags of mail, they’re organizing themselves. When the window comes up to sell you the stamps or to accept your mail, there’s really a lot less action going on. So, he basically said, the brain is talking to itself all the time when it’s resting, when it’s sleeping, and we must be able to tell the difference between the way the brain speaks to itself when you have ADHD or when you have depression or if you’re a typical, normal patient, or subject.
And therefore he has been able to find a section of the brain where you can actually see a difference that he hypothesizes has to do with attention and one with cognition and with mood. And what he’s trying to do by collaborating with people all over the world and getting data, whether someone has autism or children who have ADHD, is to really start building curves. So that when you take your child to the pediatrician and they take a height and a weight, it’s meaningless unless you can put it on a curve. So if your child has always been very skinny and has always been on the 25th percentile, that gives you some reassurance that the child is moving along, if your child becomes very fat all of a sudden and is now in the 75th percentile, the physician is worried as to how that is different.
If we could produce curves of what the trajectory would look like for a child with autism, or a child with ADHD or depression, when a patient would come into the office who seems very inattentive, seems impulsive by history, seems hyperactive and you’re not sure that if you were able to be able to do a resting state with a functional MRI, and the child doesn’t come on that curve of ADHD, you might say, "Well, there’s another reason. Maybe its parents are fighting; maybe it’s a boring teacher." There’s endless reasons why someone could be inattentive and impulsive. But if they have that history and they have that biological marker, that’s more evidence and gives more confidence to the ability to make a diagnosis. And the earlier we are able to make these diagnoses, we certainly know—considering how the plasticity of the brain—we are quite convinced that we’ll get better treatments and be able to let kids have much better lives.
We have 15 million children in the United States today that have a psychiatric disorder. The overwhelming majority never get any help. And what usually happens to them is that they drop out of school, they get in trouble with the law and they go to jail. There are 7,000 child psychiatrists. There are 3,000 individuals who identify themselves as child psychologists. So the math doesn’t work. So unless we are able to figure out a better way of diagnosis with more confidence and are able to teach pediatricians how to diagnose and evaluate and possibly treat, or nurse practitioners, or social workers to do this in a more systematic way, we will continue to lose many, many kids to the bad outcomes that happen when you have these disorders.
Recorded August 18, 2010
Interviewed by Max Miller