Antibiotic Resistance is a Growing Problem. Have We Just Figured Out How to Stop It?

When penicillin was discovered growing on a Petri mold by Scottish scientist Alexander Fleming in 1928, he mostly neglected it for a decade. The few therapeutic attempts were unsuccessful. Then a series of bacterial outbreaks occurred during World War II. Oxford pathology professor Howard Florey chose penicillin as a potential medicine. It worked.
Florey’s first patient was an Oxford policeman infected with staphylococcus, which occurred when he was punctured by a rose bush. Not enough penicillin was used; the officer soon died. Going back to the drawing board Florey and his team eventually transformed medicine.
Penicillin was touted as a miracle drug when first introduced to the public in 1945. Just as quickly, however, bacteria grew wise to this offending agent. Resistant strains popped up, so researchers developed new strains to combat these bad actors. Numerous strains of penicillin were introduced. Streptomycin and cortisone came on the scene. In the sixties dopamine woke sufferers of encephalitis lethargica that had been in comas for decades. It turns out medicine’s golden era originated in a moldy dish.
Today many antibiotic-resistant strains emerge in the very place exerting so much energy to combat them: hospitals. Historian William Bynum notes that the “antibiotic-rich environment” promotes mutation. He writes,
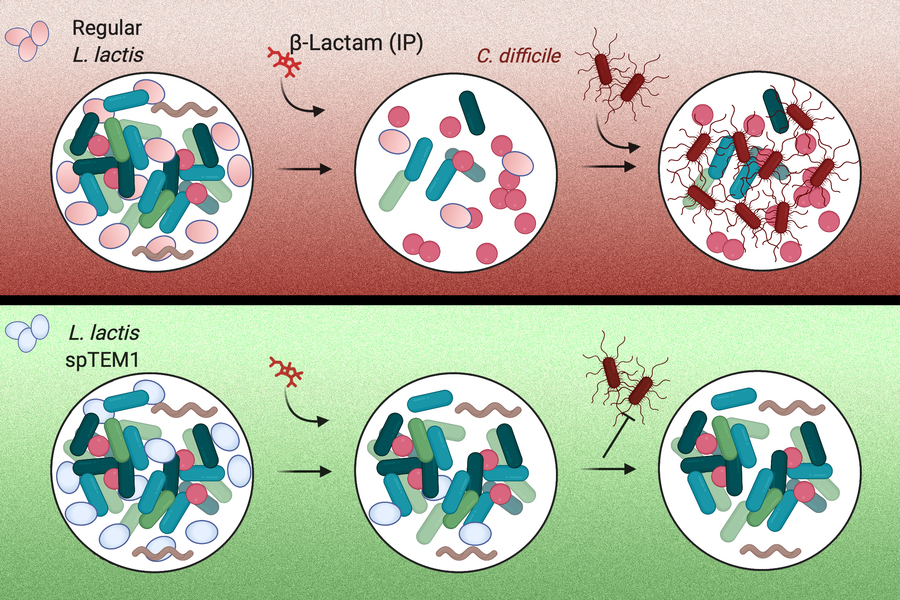
Resistance to antibiotics happens when a random genetic change in a micro-organism produces some characteristic that enables it to resist the antibiotic. In ways that Darwin would have understood, the new hereditary characteristic give the micro-organism an advantage, and it thrives.
While antibiotic resistance was not a huge concern in the 1940s, it’s become much more prevalent today. Unfortunately humans are not known for restraint. People pop azithromycin like candy. What we didn’t know during the wonder drug’s heyday was too much is definitely not beneficial. Nature relies on a system of checks and balances, and it never fails to keep its species in check.
Since researchers discovered the remarkable power—and destruction—of antibiotics, they’ve been trying to understand the mechanisms by which bacteria evolves to resist them. The World Health Organization is particularly concerned as resistance has seen a recent uptick, especially in vulnerable nations. Slowing the spread of resistant diseases has become a priority.
Florey learned early on that not only dosage but timing matters. Some courses are spread out over weeks while others require a single dose. A recent study published in Science addresses the “dormancy mechanism” bacteria are apt to develop. When woken from slumber some bacteria evolve at a rate twenty times faster than before. When this happens antibiotics are powerless.
Lead professor Nathalie Balaban at Hebrew University’s Racah Institue of Physics exposed bacteria to daily antibiotic treatment in her laboratory. Resistance was established when certain bacteria became transiently dormant:
First the bacteria evolved to “sleep” for most of the antibiotic treatment, and then this “sleeping mode” not only transiently protected them from the lethal action of the drug, but also actually worked as a stepping stone for the later acquisition of resistance factors.
Exposure, as we’ve long known, breeds tolerance. This study will guide researchers developing new antibiotics. Attacking tolerant bacteria might be the next step in prescribing a lasting course of treatment.
That patience is a virtue is as true in biology as with our emotions. While seemingly miraculous nearly a century ago, antibiotics fed our impatient attitude to disease. We want a pill for everything; we want immediate relief. As with the common cold, however, we have to wait out the onslaught of bacterial infections. In haste we’ve made a poor decision regarding healing. Now that we’re better at understanding the consequences of too much too quickly, hopefully we’ll target the real issue of bacterial infections.
—
Derek’s next book, Whole Motion: Training Your Brain and Body For Optimal Health, will be published on 7/4/17 by Carrel/Skyhorse Publishing. He is based in Los Angeles. Stay in touch on Facebook and Twitter.