A conversation with the molecular biologist at Cold Spring Harbor Laboratory.
Gregory Hannon: Greg Hannon and I’m a Professor at Cold Spring Harbor Lab.
rnQuestion: How does your lab typically operate?
rnGregory Hannon: Sure. The lab is sort of organized chaos. There are about 35 or 40 people in it. Graduate students, post-doctoral fellows, technicians, support staff, etc. We have probably an unusually broad research program. We focus in on three major areas. We work on the biology of small RNAs, we work on cancer biology, usually with the roles of the small RNAs in cancer and ways in which we can use small RNAs to understand cancer. And then we have a third area, which is technology development and genomics and mostly making use of some new generation sequencing technologies to try to understand everything from the evolution of cancer to human evolution.
rnQuestion: What is RNA interference?
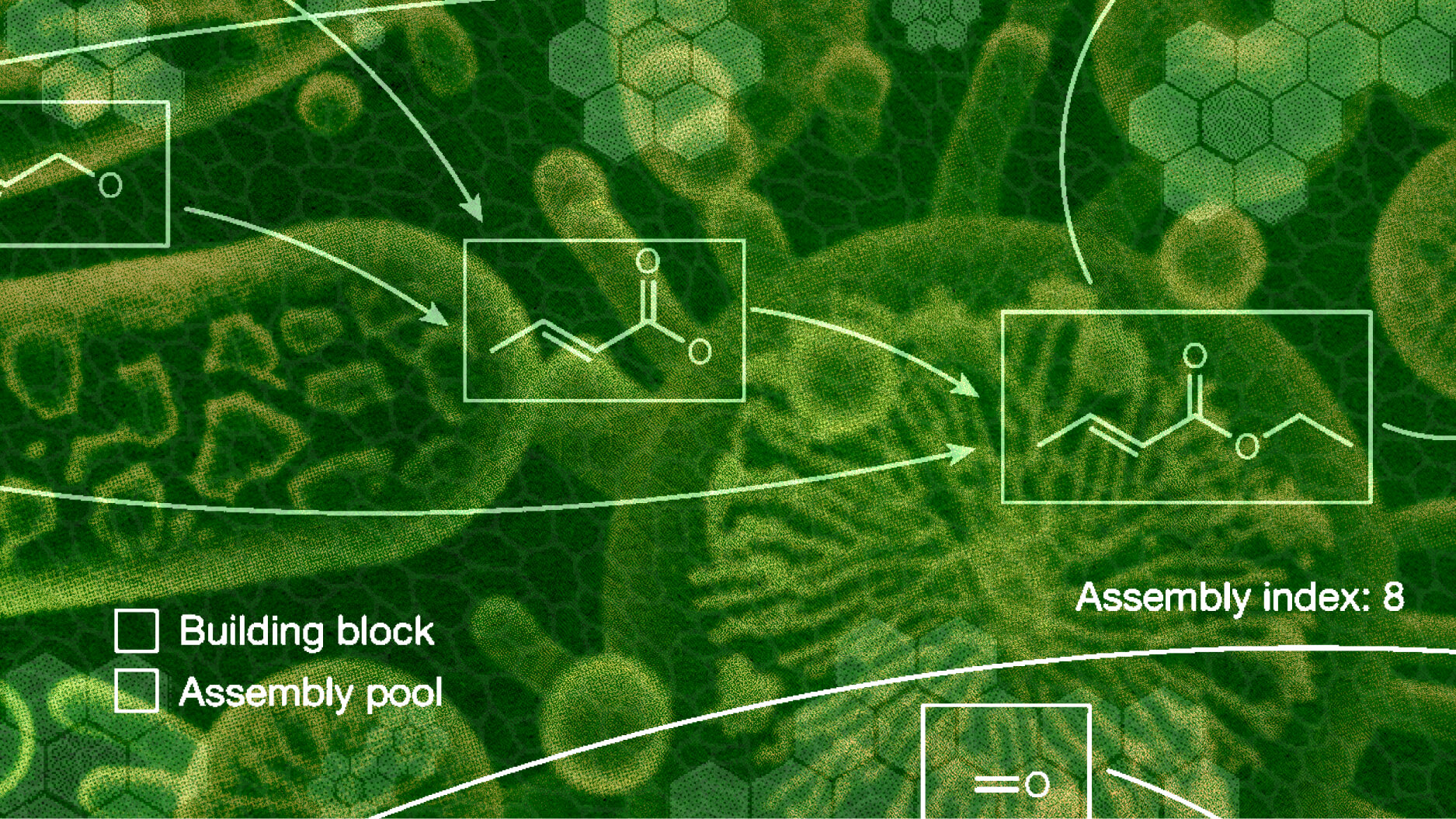
rnGregory Hannon: Well, RNA interference actually now describes a fairly broad range of biological phenomena. The notion is that RNA has a sequence just like DNA does. So then that sequence can be used to recognize complementary RNAs that share the sort of inverse of that sequence, the image of that sequence if you want to think of it that way. And through that recognition, a lot of jobs can be done. The RNAs recognized can be destroyed, they can be taken to different places in the cell, or they can even guide processes as strange as taking pieces out of the genome, depending on what organism you are talking about.
rnQuestion: How can RNA interference be used to “silence” genes in living cells?
rnGregory Hannon: The evolutionarily deepest role of RNAi is as a genome defense. It’s a way that plants, for example, recognize and fight viruses. It’s a way that animals recognize parasitic pieces of DNA within their genomes, called transposons, and shut those off. It’s also a way that the cell uses RNA to program the regulation of its own genes, and we can exploit any one of these responses, essentially tricking the RNAi machinery into silencing any gene that we want just by fooling the machinery into recognizing it as, in essence, one of these foreign elements. And we can use that for a number of purposes. The one we mainly use it for is for trying to understand the biology of those genes. And again, in our case, mostly trying to understand what different sets of genes do in tumor development.
rnQuestion: What experiments have you performed to investigate the role of the RNAi pathway in animals?
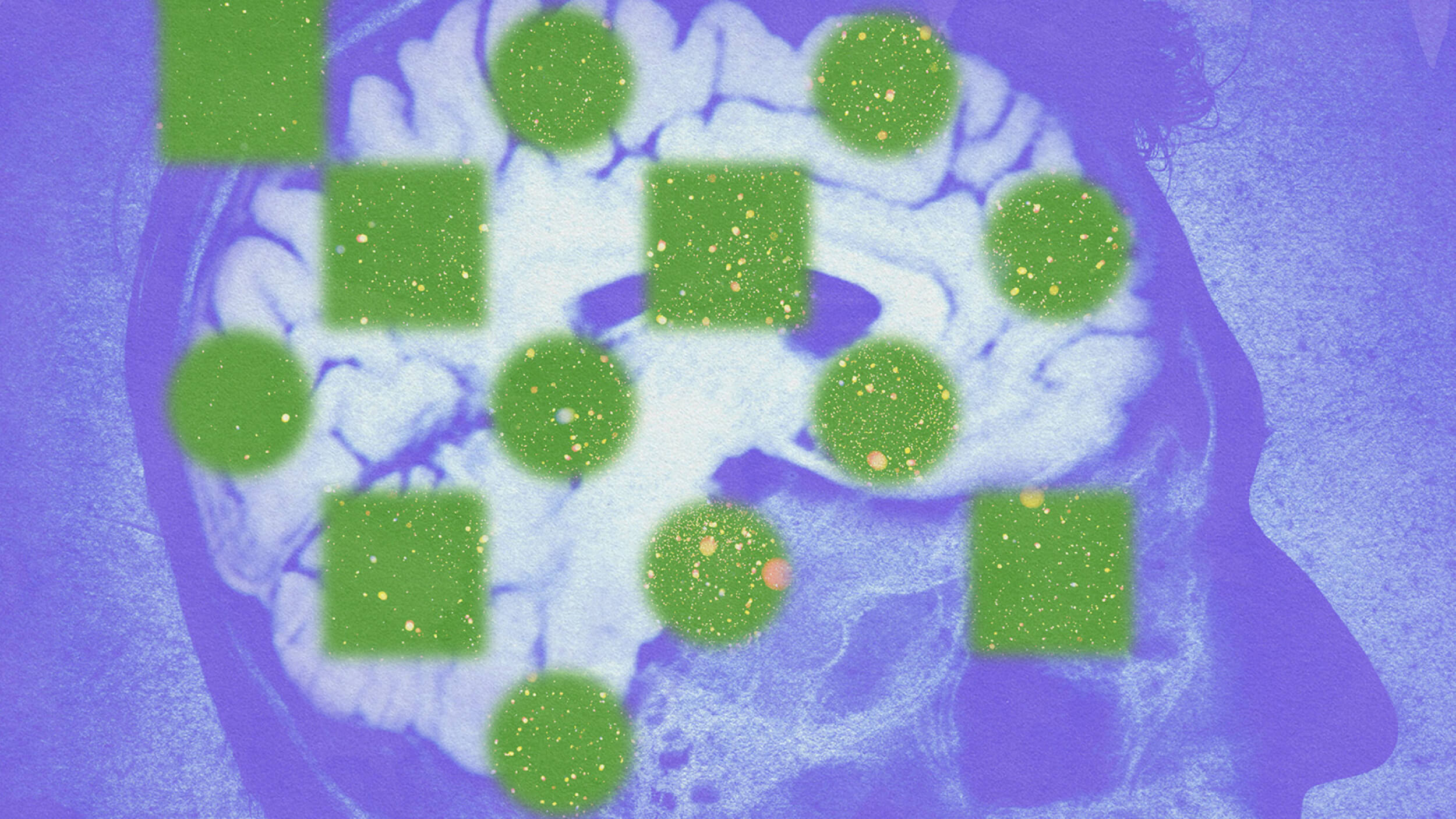
rnGregory Hannon: We’ve done a number of experiments in mice to try to figure out really, what RNAi does in animals, and I can give you a couple of examples. One is, we’ve looked at the small RNAs that the cell makes in order to regulate its own genes and compared the spectrum of those small RNAs in normal cells versus tumor cells.
rnIn one of the first cases that we did this was in a tumor type called D-cell lymphoma. And by making that comparison, we discovered that there were a set of micro-RNAs, which is what these endogenous small RNAs are called. They’re different between the normal cells and the tumor cells. It turns out that that locust, that gene which encodes those micro-RNAs is often amplified in that specific tumor type. And if we reproduce that event, adding extra copies of that micro-RNA gene, we actually accelerate the development of that particular tumor in mice.
rnAnother way we approach this problem is by taking all of the components of the RNAi machinery, all the proteins that actually bind to the small RNAs and that the small RNAs programmed to do these regulatory events and delete them from the genome and ask what the consequences are. And it was in part those experiments that led us to the realization that RNAi in animals placed this sort of genome defensive role, protecting the DNA of germ cells from the ravages of these mobile genetic elements called transposons.
rnQuestion: What are the potential applications of your RNAi studies in the field of cancer research?
rnGregory Hannon: Well, for a long time, we’ve been interested in using RNAi as a tool to silence genes of interest, whatever genes we want. And in fact, my lab has built large collections of RNAi inducing agents, in fact, collections that can be used to turn off every gene in the human **** genome. Now, the way that we use these to investigate cancer biology is essentially to take a set of cancer cells, engineer them so that each cell has a different gene turned off, and then we ask how those cells react under stress. What genes do cancer cells require that normal cells don’t? These are potential targets for therapy. What genes modify the responsive cancer cells to chemotherapeutic agents, or targeted therapies? What genes modify the ability of cancer cells to engrafted host to metastasize, etc.?
rnQuestion: What new cancer therapies might be drawn from this research?
rnGregory Hannon: Well there are really two ways that one would move from the work that we’re doing to something that would be applicable in the clinic. One is a process that is being repeated in many pharmaceutical companies. Many labs really built on the foundation of understanding this basic piece of biology, which is searching for unique vulnerabilities in tumor cells. Now, once one finds a cell upon which a particular subtype of breast cancer, for example, depends that the normal epithelial cells don’t depend on, then one can find targeted agents using standard pharmaceutical chemistry that could inhibit the activity of that particular target. And there you have a potentially selective therapy in a way that things like Gleevec are selective for specific gene rearrangement upon with the tumor cells carrying that arrangement uniquely depend.
rnAnother promise of RNAi is that it can be used as a therapy itself. And there is a tremendous interest in this, both in the academic and in the industrial communities. The notion that pharmaceutical chemistry can only access only about 20% of the genes encoded in the genome being as we have a limited ability to regulate chemically, the activity of the proteins encoded by the other 80%. RNAI doesn’t have such a limitation. All it needs to be able to do is to specifically recognize the sequence of that gene in order to shut it off. And so it is essentially, in some ways, a potentially universal pharmaceutical approach. The difficulty is, and I think this is where many of us are focusing a lot of effort, is trying to figure out how to take this relatively large molecule compared to a normal pharmaceutical and get it efficiently delivered to the cells in which the therapy needs to operate.
rnAnd so really, that is one of the major barriers to taking this basic science discovery and really exploiting it as a tool for improving human health.
rnQuestion: How do you foresee this molecular delivery barrier being overcome?
rnGregory Hannon: Well, I think that the way this barrier to delivery will be overcome is chemistry. So, it’s clear that we’ve pushed the biology of RNAI as a silencing tool sufficiently far that, given an inability to deliver this, we could shut off any gene that we wanted to and in fact, we could probably dial the activity of these inhibitors to the point that we could even figure out exactly how far down we have to turn a gene. Maybe you don’t want to shut it off because maybe it’s essential. Maybe you want to inhibit its activity 50% or 80%, and the tools **** in the biology is sufficient that we can achieve that with the tools that we have.
rnI think we will see advances in delivery come from is in changing the chemistry of the small RNA itself sufficiently that it can pass through cell membranes without the aid of a specific delivery agent. Delivery agents are the other arm of research into RNAI delivery encapsulating RNAs and lipids and polymers, and that’s another strategy for getting small RNAs into cells.
rnBut my own feeling is that the unformulated molecules probably have the best potential to be a future therapy, the simpler formulation in something where you’re mixing an RNA agent and a series, for example, of polymers, to try to get them across the cell.
rnQuestion: What insights did your research reveal into the origins of the facial cancer wiping out Tasmanian devils?
rnGregory Hannon: Well, this is, I think, an interesting story about the social aspects of science in a way. The realization that this transmissible cancer even existed came from a graduate student in my lab who happened to be Tasmanian. She did her PhD on basic aspects of RNA biology, and when she finished her degree before she moved on to a position as a post doctoral fellow, she was looking for a transition project. And she explained to me that this transmissible cancer existed that, in the last 10 years, it had wiped out roughly half of the Devil population and that it was estimated to actually drive the Devils to extinction sometime in the next 30 or so years if nothing were to be done. So, she was very passionate about his and convinced me that we had the tools to try to understand at least something about the biology of this disease.
rnNow, there are only two transmissible cancers that I know about where the cancer itself, the cancer cells themselves move from one individual to another. There’s this Tasmanian Devil facial tumor and there is also a tumor that does this in dogs. In dogs, the tumor isn’t as aggressive. It often spontaneously goes into remission and doesn’t often kill the animals that are, in essence, infected with this. In Tasmanian Devils the tumor is extremely aggressive, often kills affected animals in roughly six months with these horrific facial tumors that ultimately kill the animal often because they grow so large that the animal can no longer eat. But it’s a very aggressive disease also in the sense that it metastasizes to many sites in the body, but the animals are killed so quickly that it’s usually not the metastases that cause them to succumb as happens in many instances of human cancer.
rnSo, our basic question was really to try to understand the origins of this transmissible tumor to try to understand what cell type the tumor was derived from so that we could maybe gain some insight into to why this tumor has such an unusual etiology. And also to try to understand why it is that this tumor can spread from individual to individual, you know, is that such an unusual property?
rnWe came at it from a number of different perspectives. First, really founded upon our work on small RNAs, each cell type expresses a specific repertoire of small RNAs that it uses to regulate genes, but that repertoire is also kind of a signature of the cell type that the small RNAs is expressed in. So you can use a small RNA signature to tell a mammary cell from a germ cell. You can tell a nerve cell from a muscle cell. And so we started off by asking what spectrum of small RNAs these Devil facial tumors expressed. And that pointed us, in addition to looking at the messenger RNAs, these RNAs that encode the proteins within that cell by looking at the small RNA profiles and the messenger profiles. That really led us to a specific cell type, which in this case happens to be a Schwann cell.
rnWhat Schwann cells are is essentially like the insulation on a wire. They wrap nerve cells and act essentially as an insulator to make their conductance of signals more efficient.
rnQuestion: What course of treatment or action does this research suggest?
rnGregory Hannon: Well, I mean, I think the two things that really come out of the work that we’ve done looking both at the tumor and the host animals are that the host animals themselves are remarkably genetically homogeneous. And so, one insight that emerged from the study is that the notion that the tumors may be able to spread from animal to animal essentially like a metastasis, but within a population rather than within an organism, in part because the animals can’t recognize these cells as foreign.
rnNow, in terms of a treatment, it’s difficult to envision wild animals undergoing cancer therapy. You can’t really imagine a mobile ICU in the Tasmanian bush. But one thing that one can consider is a prophylactic therapy. And so cancer vaccines have kind of a bad rap in part because they haven’t worked particularly well for humans, but the unusual nature of the Tasmanian Devil tumor and the fact that every tumor is identical, is a very different situation than one has with human cancers where every cancer is different. It is individual not only to the person, but in its genetic composition. And so, in some cases the difficulties in developing cancer vaccines in humans might be related to the heterogeneity of the tumors, whereas when it is precisely the opposite of the situation in Tasmanian Devils.
rnSo, one can really envision two approaches; one is the approach which is being taken, which is to take a set of Devils and set them aside as an insurance population. And so you essentially sequester disease-free Devils with the idea that should the population actually go extinct in the wild, you have animals to reintroduce. Now in that case, we can use the work that we’ve done, which in essence led to a diagnostic marker for this disease, to ensure that any tumors that that insurance population might develop aren’t DFTD.
rnIn the second instance one might imagine trying to develop a vaccine against this particular unusual tumor cell that could potentially be used on wild populations, although you can imagine the challenges that one would face in doing that.
rnQuestion: What obstacles does the unique genetic composition of human cancers pose to treatment, and how can they be overcome?
rnGregory Hannon: Although each cancer is unique, there are certain core pathways, biological modules in essence, that are altered in nearly every cancer cell. And the number of those modules expands as one gets more specific to a particular subtype; let’s say estrogen receptor positive breast cancer. So, the notion, and this is one of the ways in which RNAi is being deployed very powerfully, is to try to correlate the vulnerabilities that are created by the inactivation in those individual biological models and then exploit that vulnerability for therapy. The way that you can think about this is that cells are designed or evolve to be robust. And every time you take away one of these biological modules, these pathways, it affects the robustness of cells. Think about a Jenga tower, and you’re pulling blocks out of a Jenga tower. The more blocks that you pull out, the easier it is to make that tower fall. And what people are doing with RNAi is trying to figure out precisely what additional block to pull out to make that tower fall. Where the tower wouldn’t fall if one had a normal cell which essentially has homeostatic mechanisms to be robust, to resist the biological difficulties that would be created by the loss of the pathway that would represent that key therapeutic target. So, the idea is to exploit common aspects of the genetics to create therapies that overcome the individuality of the disease.
rnQuestion: What kinds of bioethical issues arise in your work, and how do you address them?
rnGregory Hannon: In our own work, I think we encounter bioethical issues in a few different ways. One is anytime we are dealing with experiments with living animals. There are certain standards that we have to maintain about the treatment of those animals. And we also try to plan using statistical tests to make sure that we use enough animals to get a definitive answer, but no more than we actually need to do an experiment.
rnFrom the standpoint of using human materials, we encounter issues of bioethics in two different ways. They are in some ways related and I think this goes to the development of a lot of these new high-capacity technologies that are being deployed in biology at the moment. So, on one hand, anytime we use human’s samples, there are a set of rules that are in place to maintain the anonymity of patients. And so, for example, when tumor samples are collected, they are anonymized and we have no way of tracing back the material that we are analyzing to the patient that was its source.
rnThe difficulty comes as we are more and more able to sequence people’s complete genomes for reasonable cost and in a very short time. If you think about how long the human genome project took and what its cost, I mean it was astronomical, compared to today when we could conceivably sequence an entire human genome in probably a week, maybe two weeks and presently for a cost of $40,000 to $50,000. And that time it’s taking to resequence a genome and the cost of doing so is dropping continuously to the point where, really by the end of this year, it will be down to $10,000 and maybe one week. And who knows where we will be in another year or so.
rnEssentially, once you have determined that genomic sequence, there is a unique identifier, an identifier unique to that person in whom the sample was derived. Now, if we go to publish data derived from that sequence, we are obligated to put the primary – the raw data to make it available to the community. So that means that a sample has turned into a sequence which is unique to that individual, which then essentially, in some ways, public. Now for other investigators to access that, they need to have specific bioethics training, etc., but that information is out there. And although it’s not immediately connected to that person from which that sample is derived, it is in some ways eventually connectable.
rnAnd so I think that one of the places that we really struggle now is using the power of these new sequencing tools to try to understand biology and how we can do that in a way that doesn’t necessarily put the sequence of many people’s genomes essentially freely accessible on the Web. And I think this is something that a lot of people are struggling with at the moment as the sequencing technologies that I’ve mentioned become more and more widely available within the academic community. We need to establish ways to, I think at least, anonymize the information that we provide to the community without degrading the quality of the science that we do and without hampering the ability of others to analyze that data and reproduce our work, or at least verify our conclusions.
rnQuestion: Are you optimistic that patients’ genetic information can be successfully anonymized?
rnGregory Hannon: I think it will happen. A lot of it is driven – there is a sort of tug of war between maximizing people’s access to your raw information because essentially you’ve spent the money, you’ve spent the time, you’ve produced this resource, you’ve analyzed it in one way. But it could probably be analyzed in an infinite variety of ways by others. And so, you want to have people maximally be able to make use of the data you generate. And also able to, as I said, verify your conclusions. On the other hand, there is this drive to maintain privacy and in the end, what’s going to have to happen is that the community will have to establish a set of procedures that are universally acceptable to allow a sequence to remain private and anonymous without destroying the value of the data that we publish. And scientists can take a lead in this, scientific journals can take the lead in this, but it is something that we are going to face remarkably soon.
rnQuestion: What opportunities in your science education were you most grateful for?
rnGregory Hannon: Well, I came from a very small town. I had very good and very dedicated science teachers in high school who really went far beyond the call, in a way, to make additional science available after school hours, etc., doing things like science competitions that were held at local colleges, things like this and even making available some very basic college science courses during our later years of high school. Going on to undergraduate, I went to Case Western Reserve, a private university in Cleveland, with the idea that I was probably going to do medicine. The first semester I was there, I needed a job and talked to my undergraduate advisor who said, “Hey, why don’t you come to work in my lab.” And it took about a week to decide that that’s what I really wanted to do. So, for me, and I think for many, the turning point comes as an undergraduate student when you become exposed to the world of scientific research. It’s not something that a lot of people are intimately familiar with, it’s not a job that people see or encounter.
rnAnd so, I think the key opportunity is to give undergraduates the chance to come into the lab, to provide them exposure to what a life in academic sciences is really like. Graduate education is something that at Cold Spring Harbor, we’ve spent a lot of time thinking about. And really, Jim Watson pushed very hard about a decade ago to encourage us to fight against the length of graduate training, which was increasing to what he felt were ridiculous timeframes. So, a seven-year PhD of a student essentially not becoming an independent scientist until well into their 30’s was something that he thought completely inappropriate.
rnAnd so we’ve really tried to essentially reinvent graduate education in a way that allows biologists to get a PhD degree in a short amount of time; four years is our goal. We tend to meet it by and large over the ten years that our graduate program has been running; our average is about four years and three months. And in fact, I graduated a student yesterday in 3 ½ years. And so the notion of bringing people into research early and then giving them an opportunity to do independent work while they’re young and full of fire is, I think, a really critical issue that the community is trying to address.
rnQuestion: How can science improve its outreach to the general public?
rnGregory Hannon: Well, I mean, we work for the public, if you want to think about where the funding comes for our research. It comes from the National Institutes of Health, which his supported by taxpayers. And I think consequently, we have a real obligation to communicate science to the public. Outreach, I think, should happen at every level. I think that working scientists should be interfacing with high schools, for example, going into high school biology classrooms, and communicating the excitement of their work to the student. Cold Spring Harbor Lab has a very strong community outreach program, something they call the DNA Learning Center, and it’s designed to bring middle school students and high school students into laboratories and expose them to laboratory science. I think it’s our obligation as scientists to reach out to the public in the form of public lecture series. We also have a strong public lecture program at the laboratory. I participate in it and I know that many of the other investigators at the lab participate in it. And I think that the public has to understand science. Not only because they pay for it, but because science is increasingly a part of their everyday life. And to go back to the discussion of sequencing and bioethics, a time will come in the not too distant future when you walk into a doctor’s office and they sequence at least part of your genome and without a basic understanding of biology, how is the general public going to react to this. How are they going to understand what’s being communicated to them about their risk of disease and about how their own genetics affect their response to treatments?
rnQuestion: What research being conducted at Cold Spring Harbor Lab excites you the most?
rnGregory Hannon: Well, personally to me, what’s exciting about research is the moment of discovery. I think for most scientists it’s what addicts you to this; the idea that for just a few minutes you know something that nobody else in the world knows. And it doesn’t happen often because science is really a sort of an exercise in banging your head against the wall over and over again. Scientists need a very high tolerance for failure and frustration because most experiments do fail. But when something really works, and you really learn something fundamentally new, it’s something that I think I’ve never experienced in any other way.
rnRecorded on February 9, 2010