The Effects of White vs. Whole-wheat Bread May Vary Greatly Between Individuals

It’s become a convention now that when we reach for carbohydrates it is always better to choose the complex variety found in whole grain products, vegetables, and legumes. The benefits include more fiber, nutrients, and a lower glycemic response in the body (the effect the food we consume has on the levels of our blood sugar).
A new study by the Weizmann Institute published in the journal Cell Metabolism on June 6 tested the effects of whole-wheat and white bread and found that the way it was processed by the subjects was actually dependent on their individual biology, particularly the composition of their gut microbiota, rather than on the type of bread itself.
The study was a randomized crossover trial with 20 healthy subjects. For 1 week half of the participants ate industrially made white bread while the other half ate traditionally made sourdough-leavened whole-grain bread. After a two week rest period, the groups switched.
To the surprise of researchers, there were no significant differences between the effects of the two types of bread, based on multiple clinical parameters like wakeup glucose levels, levels of essential minerals, fat and cholesterol levels, kidney and liver enzymes, and several markers for inflammation and tissue damage. About half the people had a better response to the processed, white flour bread, and the other half had a better response to the whole wheat sourdough.
However, there was a statistically significant interpersonal variability in the glycemic response to different bread types. Actually, it turned out that the glycemic response to each type of bread and the way it was metabolized was person-specific and could be predicted solely based on the microbiome makeup of that person, collected prior to the study. The microbiome itself was resilient to the intervention and did not change in individuals as a result of the study.
The findings suggest that making blanket statements about a particular type of diet may not be appropriate and understanding dietary effects requires taking into account person-specific factors.
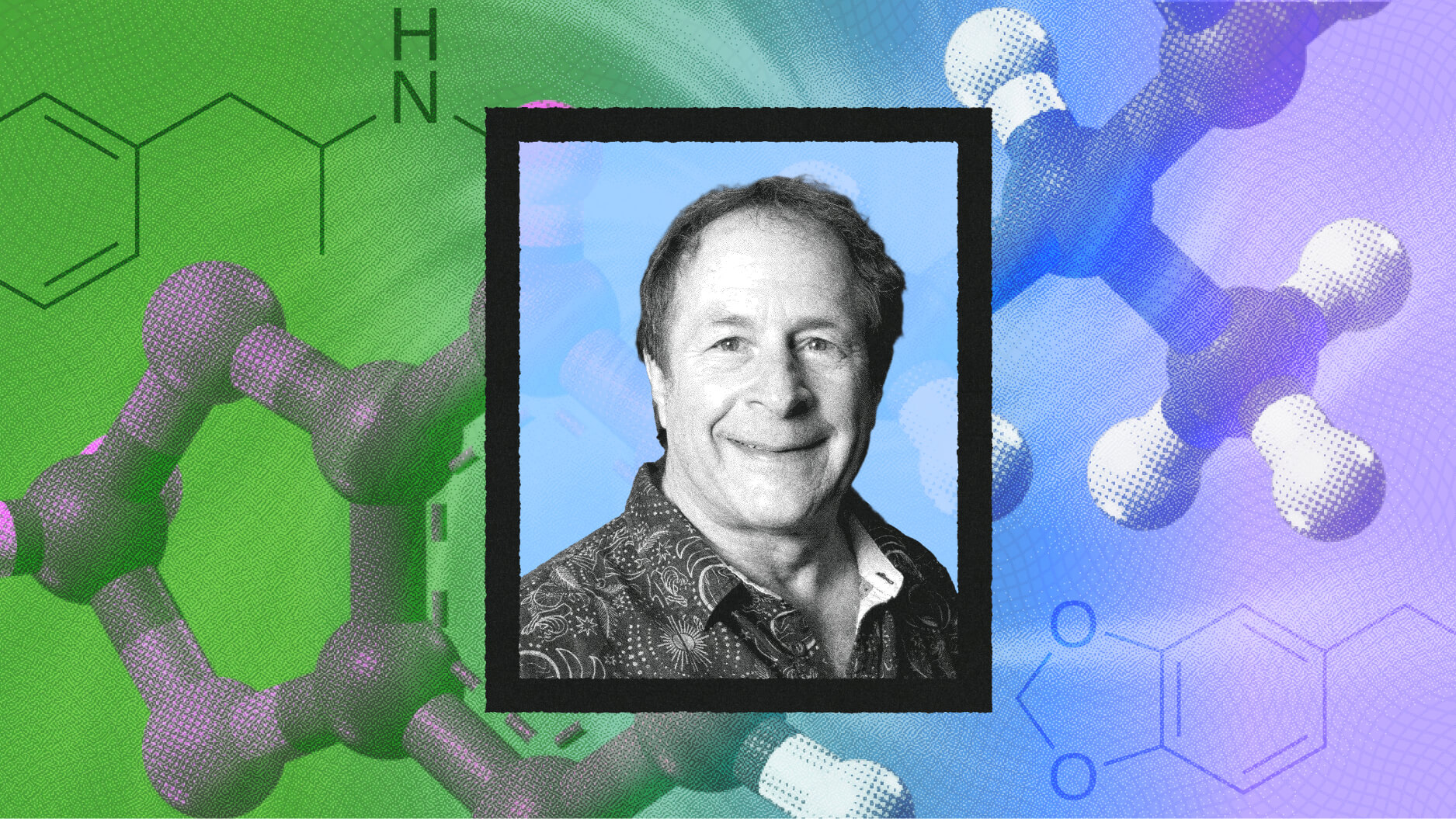
Eran Elinav, a researcher in the Department of Immunology at the Weizmann Institute and one of the study’s senior authors said:
“The findings for this study are not only fascinating but potentially very important, because they point toward a new paradigm: different people react differently, even to the same foods. To date, the nutritional values assigned to food have been based on minimal science, and one-size-fits-all diets have failed miserably. These findings could lead to a more rational approach for telling people which foods are a better fit for them, based on their microbiomes.”
The gut micriobiome is an exciting new area of study. Research has shown that the micriobiome make up varies greatly between individuals and has significant effects on the absorption of nutrients, our weight, and even our mental health and mood. Its composition starts changing from the moment we are born, based on the method of our birth, whether we were breastfed, how much we are exposed to nature and dirt, the intake of antibiotics, and what types of food we eat. Fecal transplantation is even used in some severe cases, to restore the colonic microflora and introduce healthy bacteria to the gut.
Watch this fascinating video, where Dr. Rhonda Patrick discusses how the gut microbiota affects our health withDr. Erica Sonnenburg, a senior research scientist in the Sonnenburg lab and Dr. Justin Sonnenburg, an associate professor of microbiology and immunology at Stanford.