We all feel things in our gut – intuitions that give us subtle physiological alerts, stress and anxiety that unsettle us, bad reactions to food, and conversely feelings of contentment from the right food, or flutters from an exciting experience. But according to Dr Emeran Mayer, what we feel is just a small fraction of what’s going on in a region of our body that is still quite mysterious – even to the experts.
In his new book, The Mind-Gut Connection,, Dr Mayer writes: “Your gut has capabilities that surpass all our other organs and even rival your brain. It has its own nervous system, known in scientific literature as the enteric nervous system, or ENS, and [is] often referred to in the media as the “second brain.””
As Mayer describes, this second brain consists of about 100 million nerve cells sandwiched between layers of the gut running all the way from the esophagus to the end of the large intestine. This ‘second brain’ and our regular brain use the same neurotransmitters and are connected through neural, endocrine, and immune pathways, so it truly is an integrated intelligent system with information flowing in both directions.
What makes the second brain unique from other organs is that – in animals at least – when it’s separated from the main brain it continues to pilot its complex activities on its own.
The system is extremely interesting to researchers because of this independent streak, and the effect that it may have on our mental health. After his many years of research, Mayer humbly says it’s “highly plausible” that there is a connection between the gut and mental health conditions such as depression. Scientists from the University of North Carolina have found that gut bacteria produce neurotransmitters like serotonin, dopamine and GABA, all of which have associations with our mood. Often the medications people with depression take are designed to adjust the uptake of these neurotransmitters, a treatment scientists at the time designed thinking only of the brain, but it may now also have implications in the microbiome.
What makes it even more intriguing is that more than 95% of our body’s serotonin is produced and stored in the gut in specialized enterochromaffin cells, says Dr Mayer, adding: “By far the largest store of the molecule that plays such a big role in modulating our mood and our wellbeing – also appetite, pain sensitivity – is stored in the gut.”
In recent years, the microbiome has come to the fore of scientific research, hinting at the wide reach of its sway over the body and mind. There is still a long, long way to go in understanding direct causations, but when that happens, there is no doubt our comprehension of this second brain will affect our well-being and quality of life in a big way.
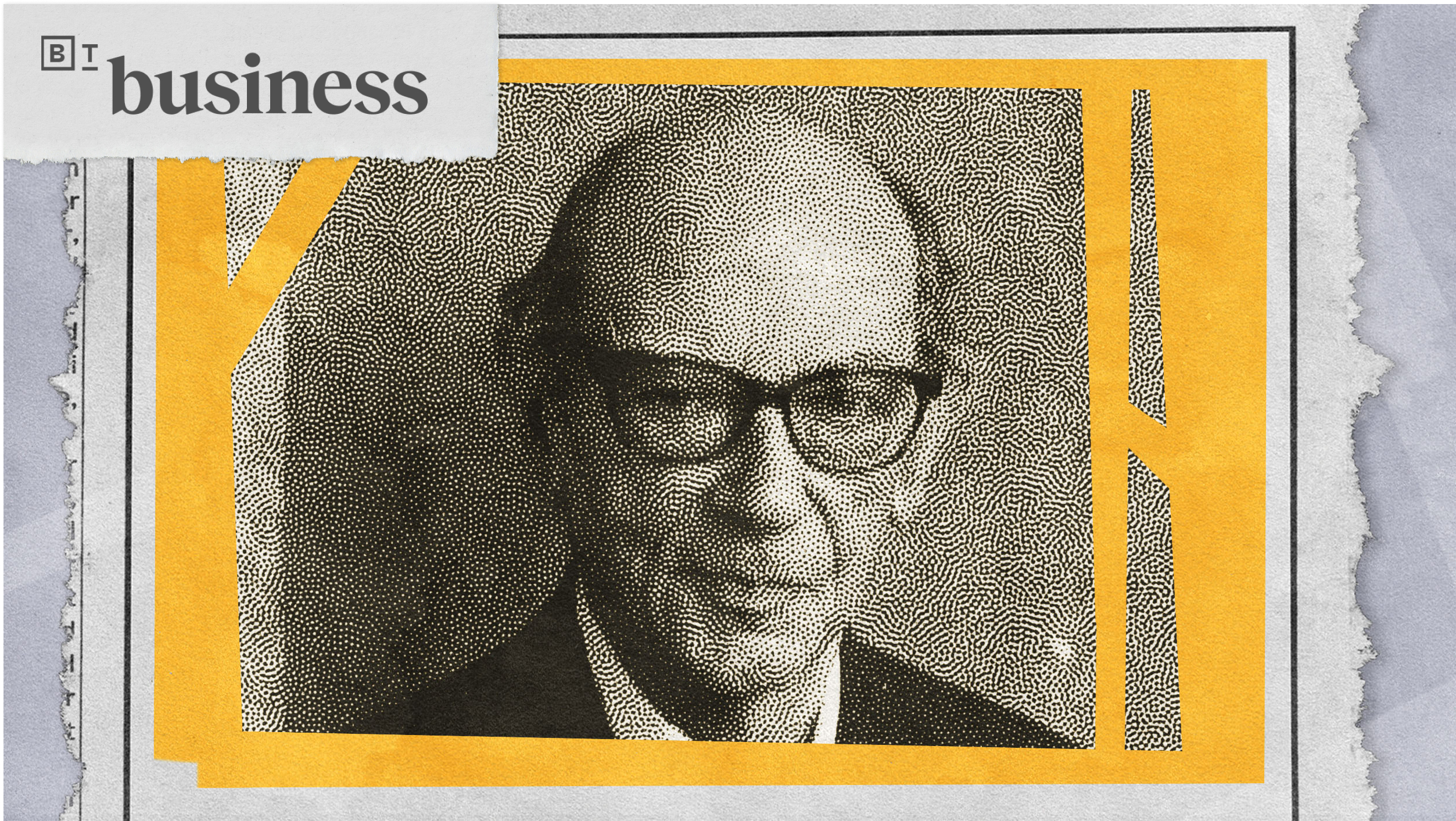
Dr Emeran Mayer’s most recent book is The Mind-Gut Connection: How the Hidden Conversation Within Our Bodies Impacts Our Mood, Our Choices, and Our Overall Health
.
Emeran Mayer: The Mind-Gut Connection is something that people have intuitively known for a long time but science has only I would say in the last few years gotten a grasp and acceptance of this concept. It essentially means that your brain has intimate connections with the gut and another entity in our gut, the second brain, which is about 100 million nerve cells that are sandwiched in between the layers of the gut. And they can do a lot of things on their own in terms of regulating our digestive processes. But there’s a very intimate conversation between that little brain, the second brain in the gut and our main brain. They use the same neurotransmitters. They’re connected by nerve pathways. And so we have really an integrated system from our brain to the little brain in the gut and it goes in both directions.
The little brain, or the second brain, in the gut you’re not able to see it because as I said it’s spread out through the entire length of the gut from your esophagus to the end of your large intestine, several layers of nerve cells interconnected. And what they do is even if you – and you can do this in animal experiments if you completely disconnect this little brain in the gut from your main brain this little brain can completely take care of all the digestive processes, the contractions, peristaltic reflex, regulation of blood flow in the intestine. And it has many sensors so it knows exactly what’s going on inside the gut, what goes on in the wall of the gut, any distention, any chemicals. All of this is being picked up by these sensory nerves, fed into the interior nervous system, the second brain. And then the second brain generates these stereotypic responses. So when you vomit, when you have diarrhea, when you have normal digestion, all of this is encoded in programs in your second brain.
What the second brain can’t do it cannot generate any conscious perceptions or gut feelings. That really is the only ability that allows us to do this and perceive all the stuff that goes on inside of us is really the big brain and the specific areas and circuits within the brain that process information that comes up from the gut. Still most of that information is not really consciously perceived. So 95 percent of all this massive amount of information coming from the gut is processed, integrated with other inputs that the brain gets from the outside, from smell, visual stimuli. And only a very small portion is then actually made conscious. So when you feel good after a meal or when you ate the wrong thing and you’re nauseated those are the few occasions where actually we realize and become aware of our gut feelings. Even though a lot of other stuff is going on in this brain-gut access all the time.
When we talk about the connection between depression and the gut there’s some very intriguing observations both clinically but also now more recently scientifically that make it highly plausible that there is an integrate connection between serotonin in the gut, serotonin in our food, depression and gut function.
On a clinical level there’s a connection because many patients with depression also complain of constipation. So a distinct dysfunction of the gut. And often the medications that people with depression take, particularly the serotonin reuptake inhibitors such as Prozac and all the other drugs in this category, they often cause transient gastrointestinal dysfunction. So that’s on the clinical level. However, what makes it particularly interesting and still an open question really more than 95 percent of all our serotonin we have in our organism is really produced and stored in the gut in specialized cells, so-called enterochromaffin cells. So our major by far the largest store of that molecule that plays such a big role in modulating our mood and our wellbeing, also appetite, pain, sensitivity is stored in the gut. And a lot of very interesting discoveries have been made more recently that makes this even more intriguing. So this serotonin is synthesized in the gut from precursors that come from our food that we ingest and the microbes that live in the gut are actually able through chemicals that they produce to stimulate the production of serotonin.
It’s been estimated based on studies in animals that 60 percent of the production is due to these signals that come from the microbes that live in our gut. So in addition another intriguing finding is that these serotonin cells, so they’re sandwiched in between the cells that make the lining of the gut. One end sticks into the inside samples, everything that goes on inside the gut. The other side very interestingly has an outgrowth which connected through a synapse with sensory nerve endings. So many vagal nerve endings. So this is a cell that sticks into the gut, samples a lot of things that go on in our digestive tract. Then it produces serotonin largely through the influence of microbes that live in our gut and then the signal when this cell is activated there’s many things chemical or mechanical stimuli associated with digestion. It signals through this synapse directly into our brain through the vagus nerve into centers that have to do with – I mean ultimately with emotional regulation and emotion generation. So even though we don’t have the proof for that it would be very difficult to mention that there’s not a significant influence on our mood and that this system if it’s out of balance does not play a significant role in the pathophysiology of depression.
There’s many food items that contain neuroreactive molecules signaling substances including oysters, chocolate and many other foods that to varying degrees contain either the precursors of serotonin or actually serotonin molecules. It’s possible that these contents of this molecule are the basis for some of these claimed effects of food items like oysters as an aphrodisiac or mood enhancer like with chocolate. People say they feel a lot better after they eat their daily piece of chocolate in the evening which is pretty true. Not just from the taste but from this chemical connection.