The future of health care could hinge on what Daniel Kraft calls “smart disease management,” the operative word being “smart” and referring to innovative diagnostic technology. In this video, Kraft displays several examples of how 3D printing, EKG, and video games can be used to boost your health. The key goal is to pursue lots of good data to help keep track of a person’s condition. “There’s an immense amount of power in data,” says Kraft, and it’s power that can be harnessed to help keep people alive.
Daniel Kraft: One of the interesting things about healthcare today is the data is becoming unsiloed and increasingly accessible. So for example, I'm wearing right now a little patch from a company called Vital Connect underneath my shirt. It's talking to my smartphone live. And I can look at a dashboard of my data from my full-on EKG, which will show up right here and it can track the trends and hopefully my EKG looks like it's okay, if there are any cardiologist out there. I can also see data about my steps, my stress level, my position.
If I fall down and I don't get back up, the system can tell that. And this is really an intensive-care-unit-like-type-level data in what will be less than five-dollar-a -ay disposable patch, which can be useful if you're training for a marathon; if you're in a hospital and you're not on a monitored bed; if your home with a disease like heart failure. That's a lot of data. We need to learn to sift through it and pull out the signals because no physician or nurse is going to want to be liable for watching your livestreaming EKG. But is an immense amount of power and data. And we're in this era now of creating digital health exhaust, whether it's my smartwatch, this patch, my phone — it can tell a lot about me, my behaviors.
If, for example, you have a patient who's got bipolar disorder, you can tell from their phone whether they're depressed or they're manic. That can play a role in smart disease, disease management. We can take technologies like 3D printing and tune home-based prosthetics. We can print prosthetic hands for folks and legs in the developing world. Here's mini me in my pocket. It's a 3D-printed version of me. That might be interesting if I need to make a prosthetic for someone who has lost part of her face. Or I was at MIT Media Lab last week and met a young grad student who diagnosed his own brain cancer, written up in The New York Times, and used 3D printing to print a version of his tumor. He said, "Hey, you want a print of my brain tumor?" This helped his surgeons do a better job of finding it and removing it. And he was proactive. He noticed some neurologic symptoms and pushed for his own repeat MRI that helped him get diagnosed earlier.
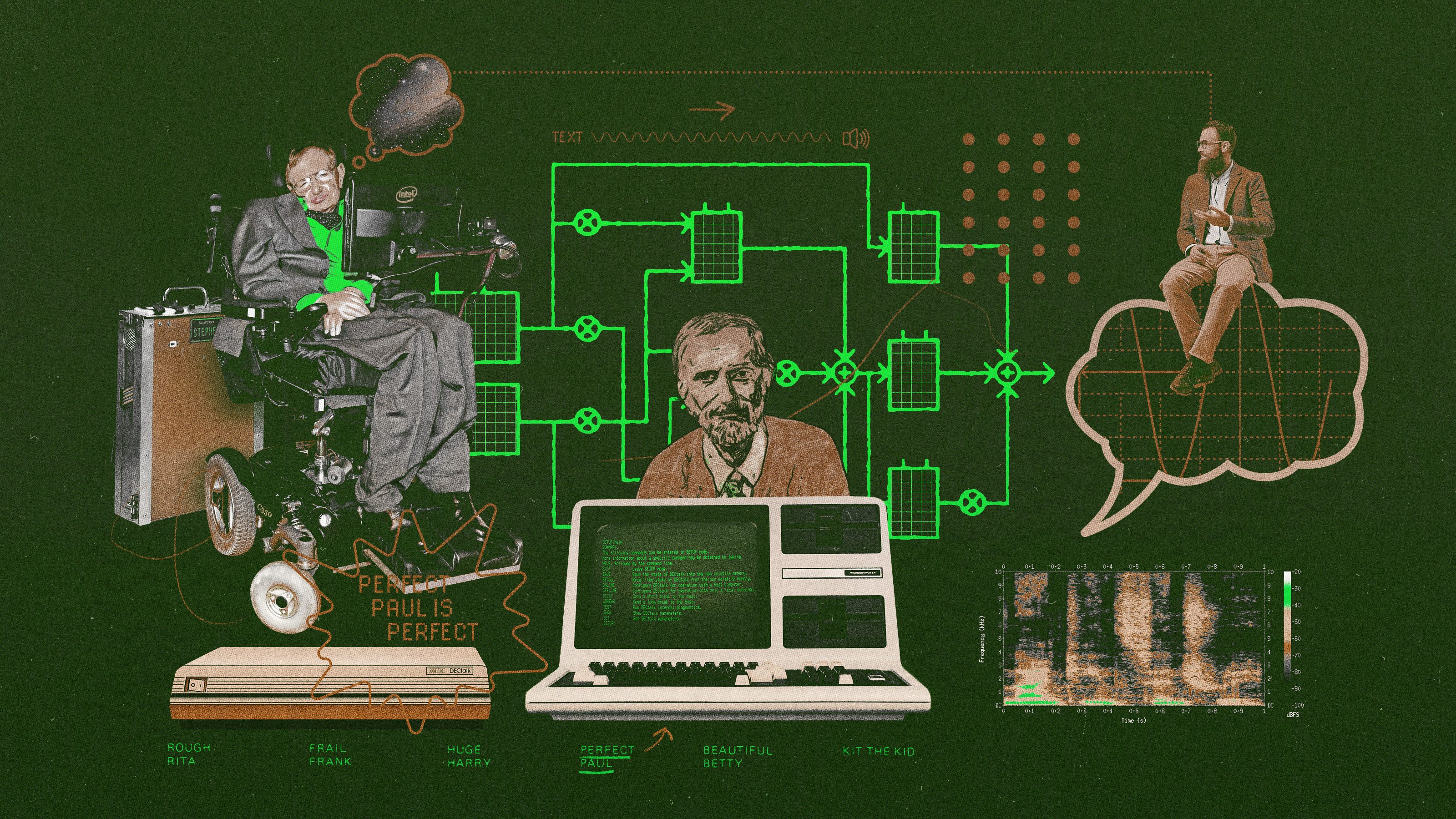
I have in my pocket a new commercialized version of a brain computer interface from a company called InteraXon. This is the Muse. You can wear this headset and kind of use this for appified mindfulness and meditation. And I might use this to prescribe to a patient who has anxiety instead of giving them a drug, I’d give them a headset. Of course they could do meditation the old-fashioned way but this enables you to quantify it, have a bit of a feedback loop. So the ability to sort of quantify our own minds with brain-computer interface like this can be used to treat everything from PTSD to ADHD. We’re going to see use of video games to improve cognition or to treat disease. We’re seeing fancy brain-computer interfaces from my alma mater Brown University to enable someone who’s quadriplegic just by thinking to move a robotic limb. And those are getting smaller and more integrated. And so the disabled in the future may just think move my arm and it will be rewired back to their own arm even if they had a spinal cord injury.
So lots of ways to take, you know, sometimes consumer devices, crowdsource new apps and platforms on these that will change neuroscience, psychiatry. And when we can pull this data together, we’ll become participatory in health care; we can move to an era kind of like with Google Maps. You donate some data when you use Waze and Google Maps — your privacy, your speed, and your location. But in exchange you can build a map of the streets and of the traffic so you get some information back. I think we can have that same sensibility in health care whether it’s sharing your brainwaves, your genomics, your wearable data while maintaining privacy and opt-in abilities. You know using that information can give us better public health, you know, early signals if it’s Ebola coming or the common flu. Or it can enable patient groups to crowdsource better cures for Crohn’s disease.
For example, there’s this new world of the microbiome. We have 10 times more bacterial cells in and on our bodies than our own human cells. We’re learning that the microbiome plays a role in everything from obesity to inflammatory bowel disease like Crohn’s disease. Maybe even some psychiatric disorders. And we’re starting to be in this era of fecal transplants. And you can imagine in five, 10 years you’re going to get a tuned cocktail of a probiotic that’s going to reboot your GI system to help treat diseases or prevent them. So, a lot of these tools are going to enable the clinician. You're going to be going to your corner pharmacy in many cases to get medical care or telemedicine.
It's going to enable you as an individual to own your own health information. There's already thousands of apps out there; some are better than others, but you can use those as tools to stay engaged in taking your vitamins and your aspirin or being on top of a much more complex regiment. And the challenge for all of us is to integrate these in the culture of health and medicine. You can have the best technology, but unless your clinician uses it and gets paid for it in some cases, it may never be adopted. The payers of the world need to start looking at how some of these can provide better outcomes at lower costs. And even before they're FDA approved, bringing these to market. And I think we're seeing many smart pharma companies, payers, physician groups think about how they layer these in to be the disruptor and not the disruptee.