New Research Suggests an Unlikely Treatment for PTSD: Antibiotics

With each passing day, the world provides us with grim reminders of a growing public health crisis. Society used to brush it off as a “case of the nerves”, before labeling it as “shell shock”, but today we know it as post-traumatic stress disorder (PTSD).
As with various other other mental health disorders, after decades of intense study we’ve greatly expanded our collective understanding of PTSD. We now know that PTSD is a psychiatric condition generated by an individual’s exposure to traumatic events, one which manifests itself through a plethora of anxiety-related symptoms.
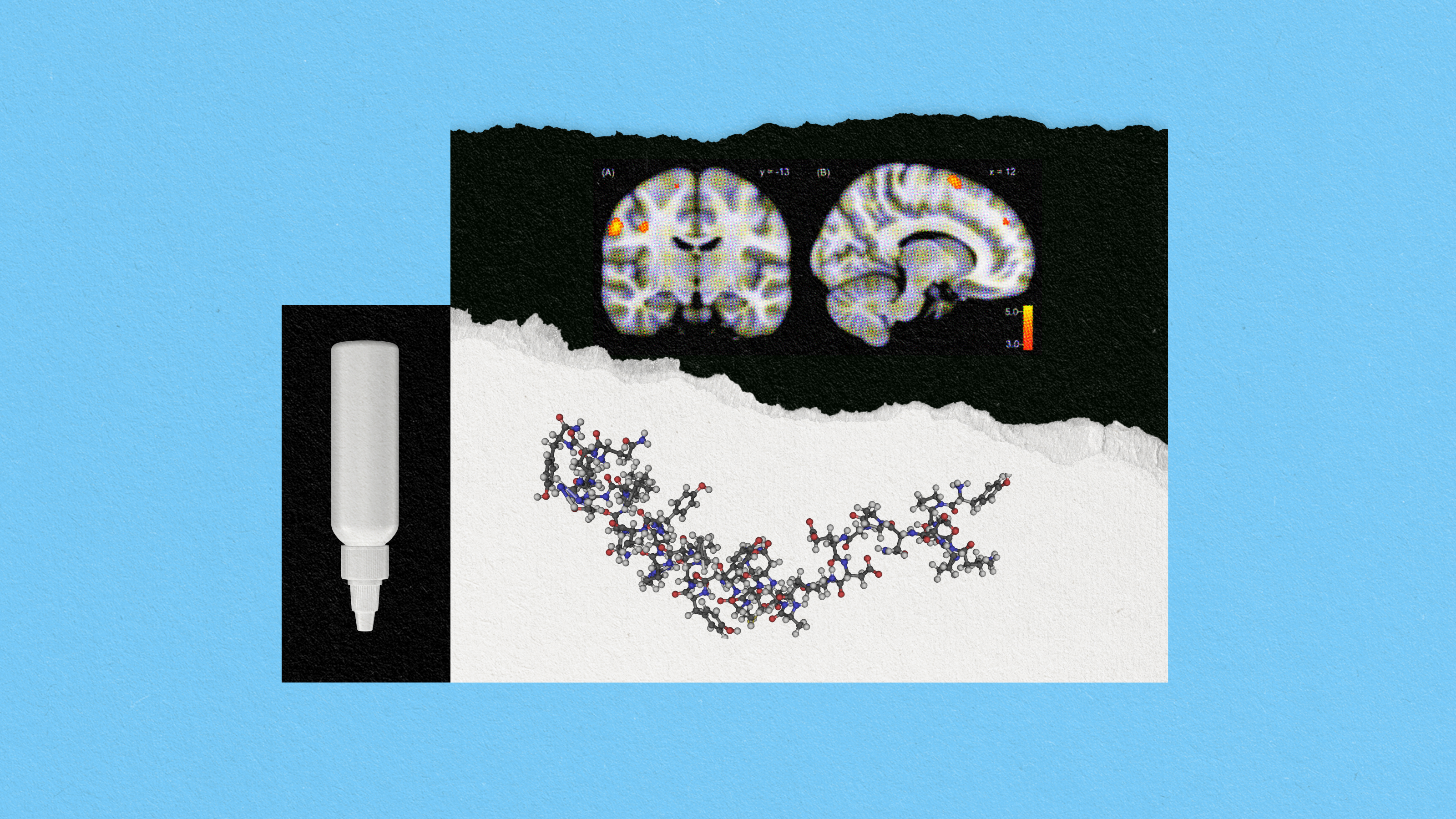
While our societal and clinical knowledge of PTSD has increased exponentially, our ability to diagnose and treat the disorder hasn’t necessarily kept the same pace. Yet a recent study conducted by British and Swiss researchers has yielded an unlikely potential treatment for PTSD, a common antibiotic called doxycycline.
In the study, researchers gave 76 healthy adult subjects either doxycycline or a placebo, then sat them in front of a computer screen that randomly flashed two colors, red and blue. The appearance of one color was associated with a 50% risk of receiving a painful electric shock. After 160 flashes, the study’s subjects grew to identify one color with the painful shocks. One week later, the experiment was conducted again with the same subjects, this time without either the doxycycline or placebo. The researchers found that the subjects given doxycycline exhibited a 60% lower fear response than those given the placebo.
Professor Dominik Bach, one of the study’s lead researchers, commented: “Learning to fear threats is an important ability … helping us to avoid dangers. (But) over-prediction of threat can cause tremendous suffering and distress in anxiety disorders such as PTSD.” He stated that doxycycline is able to block matrix enzymes, proteins that the brain uses to form memories, which explains why the antibiotic may prove to be an effective treatment in the fight against a disorder caused by an overactive fear memory.
“When we talk about reducing fear memory, we are not talking about deleting the memory of what actually happened,” explains Bach. “The participants may not forget that they received a shock when the screen was red, but they ‘forget’ to be instinctively scared when they next see a red screen.”
This is an exceptional forward leap in the theoretical treatment of PTSD. However, this complicated disorder remains firmly gripped by stigma, making its diagnosis particularly problematic.
The U.S. Department of Veterans Affairs estimates that between 7–8% of the adult U.S. population will experience PTSD at some point in their lives, yet there are certain career sectors that possess a demonstrably increased incidence of PTSD among their practitioners. For example, data from the National Center for PTSD suggests that 11–20% of Operation Iraqi Freedom and Operation Enduring Freedom veterans will suffer from PTSD in a given year. Additionally, a recent report issued by the International Association of Fire Fighters states that 20% of firefighters and paramedics have PTSD.
While soldiers and first responders are but two—albeit sizeable—slices of society, they accurately demonstrate the extent to which stigma negatively affects the successful diagnosis of PTSD. Both are not only gritty professions whose members are routinely subjected to repeated psychological trauma, but are industries in which stoicism in the face of carnage has been effectively institutionalized.
In a recent episode of PBS NewsHour, retired Green Beret, Sgt. 1st Class Michael Rodriguez highlighted both the inherent barriers to PTSD diagnosis and the acute need for new diagnostic technologies. He stated, “At that time, I didn’t think I had it. Bought into the stigma. But if there was a tangible test, I think it would make it easier on the patients, but — because it will validate it. You know, like if someone has leukemia, no one ever says, you don’t have leukemia.”
It’s here that modern science might be able to provide a modicum of relief. Dr. Sam McLean, an emergency medicine physician and anesthesiologist at the University of North Carolina at Chapel Hill, is working to identify PTSD’s biological markers through the examination of blood samples in the hopes of developing a lab-based test for diagnosing the disorder. McLean explained the rationale for his research stating, “after a traumatic event, the brain communicates with the body via the blood”.
Experts agree that we’re likely still years away from ushering these diagnostic methodologies and treatments out of research facilities and into clinics. However, it’s incredibly heartening to know that we’ve not only brought the deadly epidemic of PTSD out of the proverbial shadows, but are aggressively pursuing advances poised to subdue it.