Fauci talks about how far we’ve come since the earliest days of the AIDS epidemic, and how far we have to go.
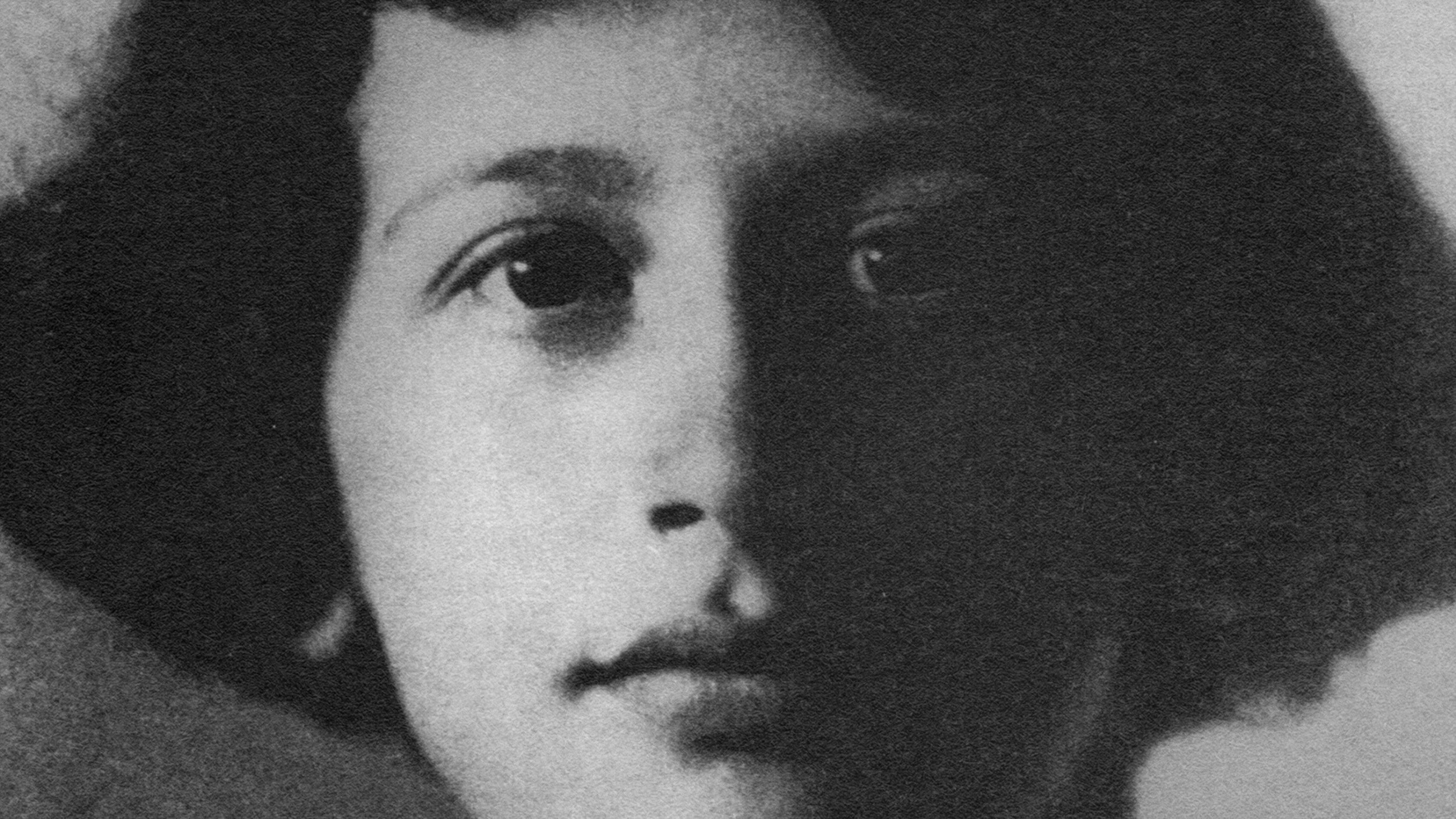
Question: How have you shaped AIDS research?
Anthony Fauci: I run a modest-sized laboratory that’s looking specifically at what we call the pathogenic mechanisms of HIV disease, or AIDS. And I’ve been doing that literally from the very first weeks of the AIDS epidemic when we first realized we were dealing with a new disease in the summer of 1981.
I can recall the very first years of the HIV/AIDS epidemic from the first patients that we admitted to our hospital in 1981, until the first drug was developed – AZT [azidothymidine] – in 1985, ’86 and early ’87. It’s that we were in a very, very difficulty psychological position where virtually all of our patients died. And when you’re a physician, like I am, who’s an infectious disease doc who’s used to curing people. Because you know, when you get somebody who’s sick, they look very sick. They’re otherwise young and healthy. You treat them with an antibiotic and you take good care of them, they get better and you get a phenomenal feeling of gratification that you’ve really saved someone’s life and you turned it around.
For the first several years with HIV/AIDS, it was very dark years because everyone who we took care of ultimately died. Then over a period from 1986, ’87 up through around mid-1990s, 1995, 1996, when the combination – what they call the cocktail of anti-HIV drugs – became available, there was an almost miraculous turnaround in the results of treating people with HIV where people would otherwise waste away and die before your very eyes, were now getting back to leading normal lives.
So that story of the interval between the early 1980s ‘til the mid-1990s really runs the spectrum of the dark years of great discouragement – of saying, “Oh my goodness. Every day I go to work and everybody that I’m taking care of ultimately dies” – to the hints of a good possibility that something good was happening from the mid-80s to the early ‘90s when drugs were coming along, but not quite the right combination until we got to the mid ‘90s. Up until today when the drugs that we have now, and the combinations have completely transformed how we take care of HIV-infected individuals.
So it’s been a very interesting journey with very, very high peaks and very, very low valleys.
During the early years of the AIDS epidemic [circa 1981] when there was a lot of activists, pain, and concern about whether the [US] government was paying enough attention to them.
And for the most part, government officials, because of the confrontational nature of how the activists were trying to get what their concerns were heard by the FDA, by the federal government, by the Department of Health and Human Services, and even the NIH, they would be very confrontative [sic]. And that confrontational demeanor was met with the reflex of staying away from them and that they must be doing something wrong.
What I decided to do back in those days was learn a lot about what it is they were saying, and finding out it doesn’t make any sense. And in fact, it turned out that it made a lot of sense. And what they were asking for was imminently reasonable.
One of the things that I’m most proud of is something that is on the border between policy and science. And that is that a few years ago, in 2002, when we had the drugs available in the developed world to have a major transforming impact on HIV/AIDS, we started to question what could be done in the developing world – particularly Sub Saharan Africa and the Caribbean. And Tommy Thompson and I were sent to Sub Saharan African countries by President [George W.] Bush to look around and come back with a proposal of how the United States government might help in the arena of HIV/AIDS to those countries that are poor and don’t have the resources that we do.
And we came back with a proposal first to try and block mother to child transmission of HIV. We presented it to the President and his closest advisors. They accepted it.
But then they said they wanted to do something even much more broad than that with a much greater impact. And I spent a lot of time on that – probably about six or seven months of my life working hard on that, which was well worth it – to put together a program of how we can get drugs, prevention, and care to millions of people in Sub Saharan Africa and the Caribbean. And we worked on it, presented it to the President, and with a lot of help from a lot people inside government, outside of government, faith-based organizations, advisors to the President, and people who really cared about it who were able to get the program to be accepted by the President, and to put it into effect by law. And that is the President’s Emergency Plan for AIDS Relief – or PEPFAR – which started out as a $15 billion dollar program over five years, which the president has now doubled to a $30 billion dollar program for the next five years, to aim at preventing millions of infections, treating millions of people, and caring for people.
It has been a huge success.
The fact that I played a role in getting the thing developed, established and implemented is something that I feel very good about.
Disease in this country, we still have a problem with HIV/AIDS. Right now there are still 40,000 new infections each year in our nation. That has plateaued [sic] at 40,000 for the last 14 years. That’s disgraceful. We’ve got to do something about that.
And the CDC [Centers for Disease Control and Prevention] is already going in that direction by making testing for HIV a part of routine healthcare.
There are a million people who are infected in this country with HIV, at least 25% of which do not know that they are infected. And the much greater majority of those people are the ones that are inadvertently transmitting the infection to others. So we’ve got to get and break that wall, and push down that wall of 40,000 new infections each year from the standpoint of health in this country. That’s, to me, the first thing that we need to do.
Recorded On: July 6, 2007