‘Upstreamism’: Your zip code affects your health as much as genetics

- Upstreamism tasks health care professionals to combat unhealthy social and cultural influences that exist outside — or upstream — of medical facilities.
- Patients from low-income neighborhoods are most at risk of negative health impacts.
- Thankfully, health care professionals are not alone. Upstreamism is increasingly part of our cultural consciousness.
If you encounter the word “miasma” today, it’s probably in reference to the worst level of a popular video game. But as late as the 19th century, medical science treated such “bad air” seriously. Under the purview of miasma theory, doctors believed that epidemics of diseases such as cholera and bubonic plague originated from noxious air wafting from decaying, rotting flesh.
Enter John Snow. Mapping an 1854 outbreak of cholera, Snow discovered that the afflicted shared a common environmental link. They all secured water from a pump on Broad Street in Soho, London. Snow theorized it was the water, not the miasmatic air, that caused the outbreak. He removed the pump’s handle, nullified the spread of the disease, and proved his theory accurate.
Because of this, Snow is widely considered the father of epidemiology. Michael J. Dowling, president and CEO of Northwell Health, offers an additional honorific. He cites Snow as a “classic upstreamist,” one whose example is important to understanding our struggles with upstreamism today.
A clinician checks a young girl’s vitals. Health care professionals do their best when the patient is with them, but patients spend much more time in their “upstream environment.”
Upstreamism is a call for health care professionals to recognize that many of the determinants affecting a patient’s health exist outside the medical facility — that is, upstream of it.
A clinician can prescribe medicine or offer advice when the patient is in their practice, but consider how much time the average person spends in a hospital and the like. Very little. Instead, the vast majority of a patient’s life is spent upstream, in their environment, where many mental and physical health issues can manifest and potentially worsen.
If a health care professional is to be an upstreamist, they must equip themselves to assess and address these social and cultural determinants together with a patient’s symptoms.
Rishi Manchanda, founder of HealthBegins and upstreamism advocate, says that “one’s zip code matters more than your genetic code.” In fact, he points out, epigenetics shows us that our zip codes can shape our genetic codes.
In his TED talk, Manchanda illustrates upstreamism with an anecdote about a patient named Veronica. Veronica suffered chronic, debilitating headaches. She had visited emergency rooms three times before trying Manchanda’s clinic. The previous doctors looked at Veronica’s symptoms in isolation, saw nothing wrong, and prescribed standard pain medication.
He measured the same vital signs, got the same results, but asked an additional question: what were her living conditions like? Turns out, her living conditions weren’t ideal. Her housing had mold, water leaks, and cockroaches. Manchanda theorized that her condition may be the result of an allergic reaction to the mold, a diagnosis the others missed because they only considered Veronica’s symptoms in isolation. They forgot to look upstream.

Volunteers beautify a park in Bowie, MD, as part of a three-year project to repair low-income neighborhoods in the county. (Photo: Staff Sgt. Alexandre Montes/U.S. Air Force)
Like an actual river, a patient’s upstream environment doesn’t flow in a straight line. In lieu of springs, streams, headwaters, and tributaries, a patient’s constitutional watershed contains their social environment, their physical environment, their economic status, their individual lifestyle, and their access to care.
As a result, people living in low-income neighborhoods face far more negative social and cultural health influences than those living in wealthier areas. Patients from such environments are less likely to have access to pollutant-free water, full-service grocery stores and farmers markets, and parks and playgrounds. The stress of such environments leads to higher rates of depression, unresponsive parenting practices, and even increased rates of mortality.
“If you’re living in a very, very good neighborhood, […] you will live years longer than the person who lives in a very, very poor area, in general,” Dowling said in an interview. “So if I want to improve your health, I’ve got to make sure that I have doctors, and nurses, etc., to provide medical care to you. But I’ve also got to figure out how to work on all of these other things.”
That’s a lot for health care professionals to be responsible for, especially when one factors in the exorbitant rates of burnout facing doctors and physicians.
Why health care should start long before you reach the hospitalcontent.jwplatform.com
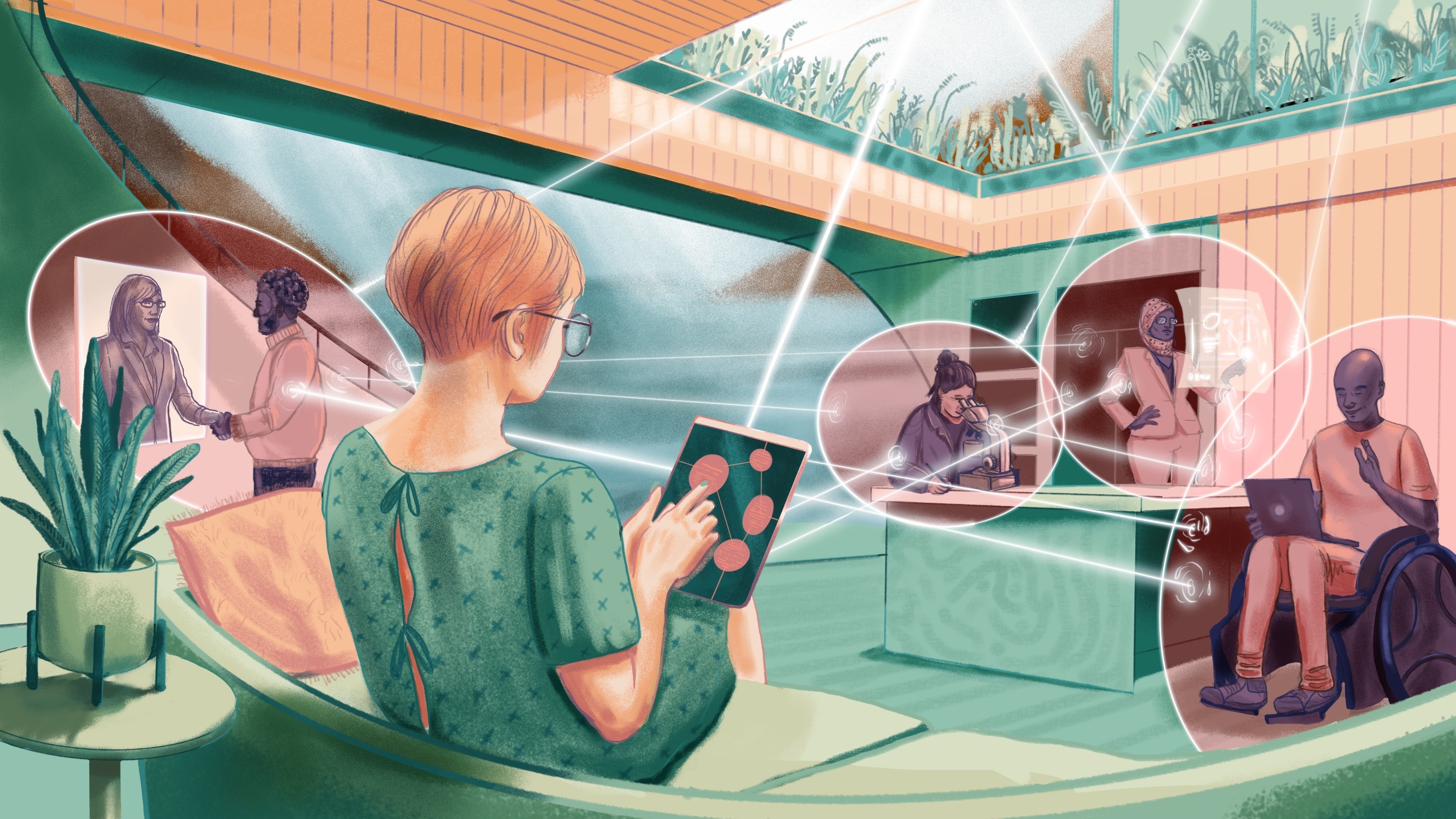
The challenges of upstreamism would be daunting to health care professionals if they had to face them alone. However, we are in the midst of social changes that will make upstreamism viable. One of those changes is an always connected world where new information is available quickly.
Going back to Veronica’s story, Manchanda didn’t solve the problem alone. He connected her with a community health worker, and the partnership paid off. The community worker found mold, a strain Veronica was allergic to. Once her home conditions improved, Veronica’s quality of life did as well. Manchanda inadvertently helped one of her sons, too, as his asthma was exacerbated by the same mold.
“If we’re all able to do this work, doctors and healthcare systems, payers and all of us together, we’ll realize something about health. Health is not just a personal responsibility or phenomenon. Health is a common good,” Manchanda said in his TED talk.
Beyond search engines, technology companies are making a big push for health care. The tools and innovations they develop could streamline the mapping of a patient’s upstream environment. For example, devices like smartphones and Fitbits may allow patients to generate their own health records, offering doctors a proactive, up-to-date account of a patient’s environment. The growing ubiquity of such devices will also allow doctors to perform virtual health visits, giving them easy access to patients and their live-in environment.
Finally, many health care professionals and organizations are heeding the upstreamist call to use their voices to advocate for changes to harmful social influences. As part of the Greater New York Hospital Association, Northwell Health has supported actions to curb gun violence in the United States. They advocate for, among other steps, a renewed ban on assault rifles, enhanced background checks, and permitting the CDC and NIH to conduct research on gun violence.
“[G]un violence isn’t just a national tragedy, it’s also a public health crisis,” writes Dowling in his book Health Care Reboot.
This brings us back to John Snow. If he hadn’t looked to the environment, looked upstream, he may have missed a solution that saved people’s lives. The problems facing upstreamists today may require solutions more taxing than removing a water pump handle. But through technology and changes in social attitudes, they are manageable and can have a lasting impact on health care.