A panel discussion among leading experts highlighting cutting-edge autism research.
Introduction
Wilczynski: One in 110 children born in America today are diagnosed with autism. That's double the rate 10 years ago, and up 10 times from a generation ago. Autism is, by all measures, increasing dramatically.
Affecting social skills and communication, the condition is in fact a spectrum of disorders, causing a range of impairments. Some who are affected by autism can be highly functioning, including those with Asperger's syndrome. Others are severely impaired by the condition. There is much we still do not know about autism, and speculation and rumor have, at times, made it difficult to develop a clear picture of what it actually is.
Welcome to Breakthroughs: Autism, the second of a three-part Big Think series looking at three of the major diseases and disorders of our time: Alzheimer's, autism, and cancer. The series, made possible by Pfizer, focuses on cutting-edge medical innovations and our efforts to develop treatments and possibly cures.
I am Susan Wilczynski, director of the National Autism Center. I am joined today by Dr. Gerald Fischbach, who oversees the Simons Foundation Autism Research Initiative. Next is Dr. Christopher Walsh, of Children's Hospital Boston and Harvard University. And lastly, Dr. Susan Bookheimer, professor of cognitive neurosciences at UCLA.
***
What is Autism?
Wilczynski: Beginning with Dr. Fischbach, tell us as simply as possible what is autism?
Fischbach: Autism is a developmental disorder characterized by two main components: an inability to interact socially with other people with joint attention to understand other people’s thoughts. And the second component, the major component, is a real tendency to restricted interests, very narrowly focused interests and repetitive behaviors. That is just the core definition; autism reaches out in many different directions. It can be associated with language delays. It can be associated with epilepsy. It can be associated with some degree of intellectual disability, but the two core features of autism, I see, is impairments and social cognition, understanding and in restricted interests and repetitive behaviors.
Wilczynski: And how is it diagnosed?
Fischbach: Right now I think the gold standard is a clinical diagnosis, that an astute clinician interacting with a child, interviewing the parents, talking with teachers makes the diagnosis based on some standard tests and also on clinical impression and skill. There are no good tests yet, we’ll talk more about that later, that I know of for biochemical tests or imaging tests, although people are getting close and that is one of the real pushes that we’ll talk about and other objective tests. But right now the gold standard objective test is clinical judgment.
Wilczynski: Very good and I think that brings up the point that the clinicians really need to have broad experience at diagnosing individuals on the autism spectrum. Seeing one or two cases of autism or even a couple of cases of Asperger’s is often insufficient to prepare a psychologist, a developmental pediatrician or other health professional to really provide a comprehensive diagnosis. Tell me what in the brain seems to go awry to create autism spectrum disorders?
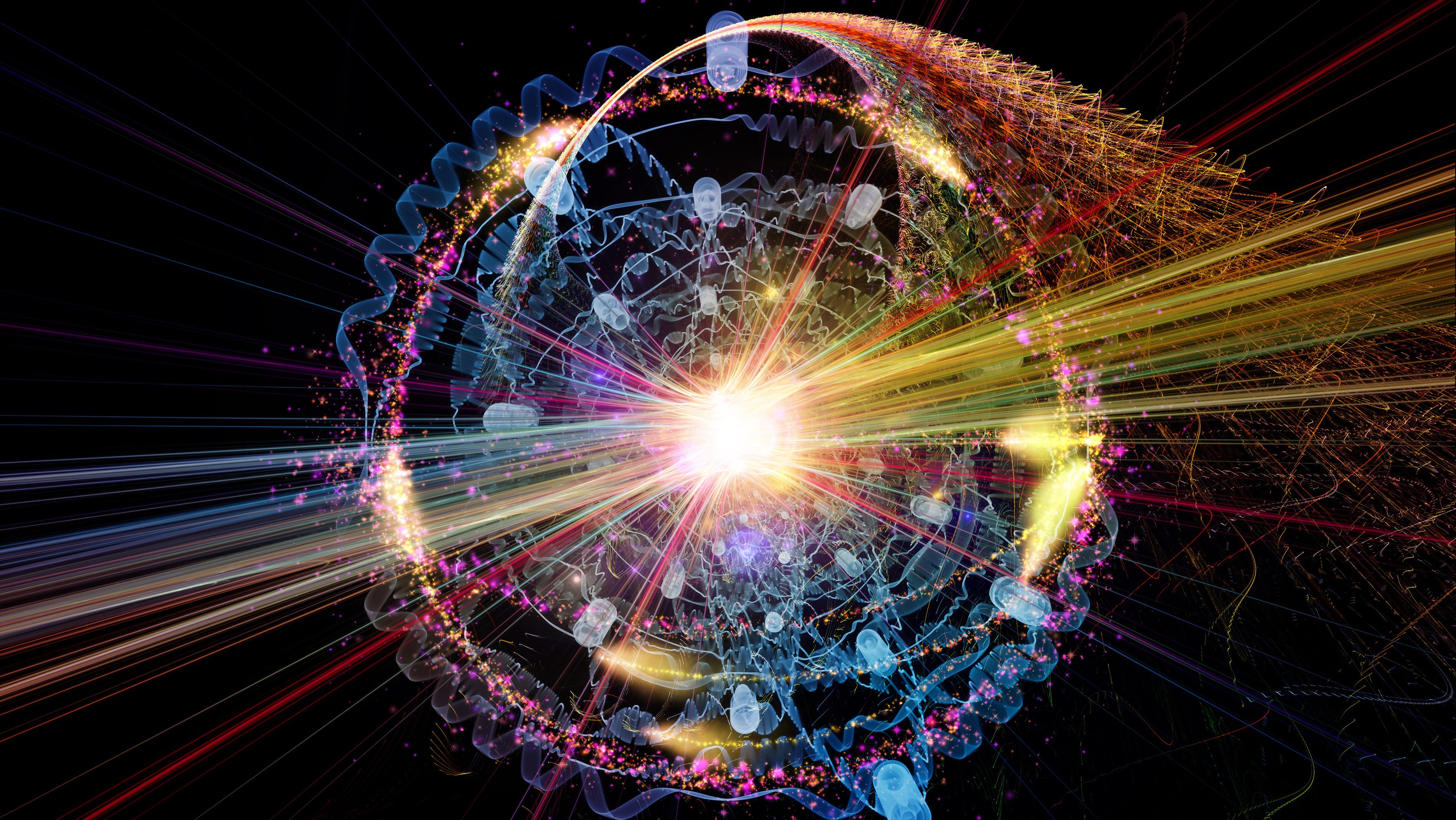
Fischbach: We just don’t know. Everyone on this panel I'm sure will have certain interests and biases and thoughts. I think my own bias is that there may be something wrong with the timing and the connectivity between regions rather than pointing to one particular spot in the brain. That it’s how these regions talk to each other and how they interact that is just not quite right.
Bookheimer: In particular I think that we’re getting closer to a model of autism that has to do with connectivity abnormalities in the brain and particularly early in development how connections are formed in the brain and, as Fischbach has pointed out, when they are formed in the brain. And in autism I think that one of the problems is that areas of the brain that are far from each other are not as well connected, whereas areas of the brain that are very close to each other seem to be over-connected. And so I think that it has to do with the developmental trajectory of when and where connections are formed that it appears to be awry.
***
Is Autism Caused By Genes or the Environment?
Wilczynski: Dr. Walsh, dozens of genetic defects have been identified and associated with autism spectrum disorders. Tell us, from your research, what have you learned about genetic roots of autism?
Walsh: Well, so far the genetic studies of autism have been leading us to much the same sorts of ideas about its root cause. You’ve already heard about this idea that there is problems with connections in the brain. Now the brain is made up of cells that have fibers connecting different parts, sort of like electrical circuits and what is unique about the brain though is that those fibers and those connections change. The fibers and the cells are the hardware, but then the brain develops different apps or different software apps for language or apps for social behavior. And it seems like it’s these patterns of changes in connections that don’t seem to work and the genetics lead us to genes that regulate these patterns of connectivity, regulate the synapses that connect one brain cell with another brain cell.
Wilczynski: Very good. What have we learned about environmental triggers for autism?
Bookheimer: So far there is not very much known about environmental triggers for autism. We know for example recently that the age of the father is related to additional autism risk. There is a recent study coming out of USC showing that exposure to small particulates, the proximity to major freeways, confers a small additional risk. But I think that those are the only two I can think of that we’re pretty sure at least associated with autism and probably don’t explain a whole lot of the increased risk of autism.
Walsh: One of the things about again the genetics leads to in terms of the mechanisms is that the sorts of genetic abnormalities that we see with autism involve these synapses and the synapses change in response to the environment. In fact, although we think that there is a large genetic component to the disease it’s by no means all genetics in the sense that the genes that are in play are those regulate the way the brain responds to the environment and so that is good news in the sense that we know that there are ways that the brain can be changed by different sorts of teaching, different sorts of environments, enriched environments and... But that also implies that that genetic predisposition is not immutable, that there might be ways it can be modified or improved.
Fischbach: Let me just amplify what Chris and Susan said about coming back to the environment at the end. What I think of when I think of the genetics of autism is two things. One, it’s complex. And two, it’s really advancing rapidly, a lot of it due to some of the work Chris has done in families in the Middle East that are now here in this country. But it’s not going to be a simple answer of one gene causes autism. In fact, what is much more likely is there may be more than 100 genes that enhance the risk of autism. There is a difference between a risk factor and a cause. There may be a few diseases we know—more than a few—where one gene causes a disease, like sickle cell anemia in Africa and more close to home, Huntington’s disease, where if you have a mutation, a certain gene you will have that disorder. In autism there is just genes in part more or less of a probability that you will have the disorder, and that is where interactions with the environment are key. Genes are not in this case, certainly not fate. You have to understand how the genes influence environment. And I think what Chris was saying was one of the important things in environment is how you learn things and that has to do with the connections between nerve cells in the brain and there are over a trillion of them. And some change right now as we’re talking to each other and some don’t change. Some are pretty... more or less fixed, but some do change. And it’s turning out that many of these genes are pointing to the biochemistry that affects these connections in the brain. That is the hope. That these genes will all converge somehow and point to one or a few targets in the brain. But it won’t be one gene.
But there are many, many ways to affect synapses, the connections, especially to affect the way synapses change with experience, so that is the hope, but first one of the primary goals is to get the cast of characters. How many genes are we talking about? Who are they and what are they pointing at? And that is when the really interesting, I think, work will begin and we’re getting close to that.
***
Why Vaccines Don’t Cause Autism
Wilczynski: In the last decade there has been a great deal of public controversy surrounding the idea that vaccines might cause autism. Where did this perception come from and tell us do you think it’s wrong and why?
Fischbach: How much time do we have? I can trace the origins of that idea and you’ll see right at the end that it’s always difficult, if not impossible, to say a concept like that is wrong. You can say that it’s unlikely or that it’s not among the prominent hypotheses today. It came... the origin I believe came from a study in England of an individual, a physician at the Royal Free Hospital who were studying children who had infections, viral infections. It seemed to disrupt their bowel habits. And he postulated that there were toxins being released from the bowel. In fact, many children come to autism clinics early on with GI/bowel disturbances. But he pointed to vaccines as causing this, that somehow it disrupted normal bodily function and caused release of toxic materials that affected the nervous system and that led to widespread suspicion.
There is a phenomenon... It is not all that common, but there is a phenomenon where autism could get worse at about age two. There are some controversies whether regression is a prominent part of autism, but many people feel that it’s very hard to diagnose autism before you can begin really talking in detail with a child. But there is some hint that some children develop normally up to age two and then go through a precipitous decline—and that is about the time they receive the measles, mumps and pertussis vaccine.
So you have two very common things, autism, 1 in 110 children some people estimate, and vaccination. And the correspondence was almost too much to ignore, especially with a troubled family looking for reasons and so the suspicion grew and then some epidemiologic studies were suggestive, but the great, great majority and millions of dollars have been spent on epidemiologic studies, have found no correspondence between vaccination and autism. It doesn’t rule it out. Nothing will rule it out until we know what the cause is.
One aspect of it that has been ruled out I believe is a preservative in the vaccine, the ethyl mercury and the mercury is put in vaccines so that the vial can be used over and over again, especially in general clinics where you have to vaccinate several children and it was thought that mercury was triggering autism and in fact, many children were treated with agents to remove mercury and other heavy metals from their system, very toxic drugs. But mercury has been removed from the vaccines since 1987. There is really... first reduced to very low levels and now essentially eliminated and the autism reported prevalence is still... hasn’t decreased. If anything, it is on the rise.
I believe the reported prevalence, and everybody should chip in, is due to wider recognition, broadening of the criteria... and you can trace this in the diagnostic and statistical manual of the American Psychiatric Association. The criteria got broader and broader and broader and more people were recognizing that their children had a slight disability. Resources became available for helping families and stigma, although it’s not gone by any means, is slightly reduced, so I think, I believe the prevalence was just as high 20 years ago, just not recognized. I don’t believe there is something that's happened in the environment, but other people...
Wilczynski: I would add to that our diagnostic tools have become much better during that period of time. Historically the professional who was providing a diagnosis relied almost exclusively on behavioral observation that wasn’t necessarily highly structured or standardized and now we have more structured interviews. We have more structured observations. And people are very careful to collect data, as you mentioned earlier, from school professionals, from parents, as well as engaging with the child themselves. And so more professionals have been educated about how to diagnose individuals and the tools we use are actually much better.
Fischbach: Absolutely right. There is a postscript to this. The original paper was written by a physician written named Andrew Wakefield, who has been debarred in England. The paper has been withdrawn. I think something like eight out of the nine authors have withdrawn their names and it’s thought to be totally fabricated, so it was based on a sham and it has not been supported and the reason I'm rather vehement about this is the danger in not vaccinating children is real.
Bookheimer: I would like to add to that. In Los Angeles Country where I live 10 children died of pertussis last year, which would normally be... would never happened. It’s unprecedented and it’s because parents are not vaccinating their children and they’re passing germs and diseases around that weren’t being passed around before and that is a direct consequence of this.
***
Do People With Autism Experience Emotions?
Wilczynski: So tell me Dr. Bookheimer, what do we know about neural dysfunction and social deficits in individuals with autism?
Bookheimer: Well we know quite a bit of small pieces of information. We really don’t know a lot about how it all fits together. That has been studied in a variety of different ways. One is looking at the structure of the brain and in looking at the structure of the brain you can’t just look at a brain scan of someone with autism and see autism in it. The brains look very normal. The consistent finding is that on average the brain size in individuals with autism is larger at least earlier in life. But if you look very carefully at that data it looks as if a minority of individuals with autism have pretty large brains and then most of the other ones are pretty much average and the differences are not so massive that it will really tell us what the problem is.
The other things that have been looked at are functional activity in the brain. When you have individuals with autism perform tasks. What areas of the brain are working, how are they working and where are some of the differences. And there, there has been a great deal of controversy. For example, one of the early findings in autism was that they didn’t seem to activate the areas of the brain that are responsible for face processing to the same degree of individuals who are typically developing. We have an area of the brain that is pretty well devoted to face processing that becomes stronger and very, very well entrenched in the brain rather early in life, and individuals with autism many of them did not seem to show that same kind of specialization. But as we’ve studied that a little bit more there have been problems with that theory. One of the biggest problems is that individuals with autism don’t tend to look at the eye region very much and when they do look at the eyes then they get more face area activity and the other I think major finding was that when individuals with autism look at people who they know very well their face areas work just fine. And so there appears to be a general difference in the way that the face area is active, but that may be a consequence of differences in social behavior and not a cause of it, which is one of the early models.
There are other brain areas that don’t seem to function as well or as typically. The amygdala, an area of the brain that is involved in the experiencing of strong and salient emotions doesn’t always react in the same way and isn’t as well regulated or modulated as it is in typically developing individuals. There are other areas of the brain that are involved in social processing all throughout the frontal cortex and in other areas of the brain and those tend to be a little bit different, less active in these social networks of the brain.
Wilczynski: You were talking about emotions and the parts of the brain that were processing emotions. Sometimes there is a perception out there that individuals on the autism spectrum really don’t experience emotions or are incapable of reading the emotions of others. Can you speak to that?
Bookheimer: Well individuals with autism certainly have emotions. I think one of the earliest findings in autism that was controversial was that individuals with autism bond with their mothers at an early stage. It was thought many years ago that they didn’t bond, but they do bond. They also have emotional experiences. Anyone who has a child with autism knows that. They get upset just like everyone else does. They may have more difficulty with some of the more subtle emotions like shame, pride, things that are much more socially oriented. But again, that might be a learning difference.
Some of us believe that one of the problems in emotional behavior in autism is simply that they’re not as well regulated and not as well integrated with areas of the brain that understand emotions and that can really think through and work through them and that is of course a consequence of being able to not just have the emotion, but to process it and understand it and understand it in context.
There is evidence that individuals with autism are not very good at reading the emotions in others. That is part of the disorder in fact. And we don’t know why that is. It may be that they’re never attending as much to others. There is a model that individuals with autism don’t seem to have the same almost innate motivation to socialize. And if you don’t socialize then you won’t learn a lot of these social behaviors including how to read other people, so we end up continuing to have the same problem: What is the cause and what is the effect? We learn a lot of how to read other people by paying attention to others and by learning through our social experiences, but if individuals with autism are spending a lot of time attending to objects and not interacting with people and not attending to people then they may not just gain that set of rules and that understanding of others that allows them to participate more in the social world as they grow older. So in a sense there is a cascading affect that occurs. An early perhaps lack of interest in others that over time will evolve because of a lack of experience in communicating with others.
***
Is Autism an Epidemic?
Wilczynski: One in every 110 children are now being diagnosed with an autism spectrum disorder. That rate is double what it was 10 years ago and really 10 times the incidence that was reported a generation ago. So what are the causes for this increase? Is it really an epidemic?
Fischbach: No, it’s not an epidemic. I believe it’s greater recognition, greater clinical acuity, more available resources and mostly a broader definition of what we mean as it blends into the normal population on the one hand and the low end of the spectrum, the intellectually impaired, on the other. As the diagnosis of autism is increasing the diagnosis of mental retardation is decreasing. And more and more on the other end, the high end, more children who are just a little bit off, who ordinarily you would not single out now are being described as perhaps Asperger’s syndrome or on the high end of the autism spectrum, so I don’t believe there is an epidemic.
Wilczynski: Very good. Anything else?
Walsh: I think in all of medicine we’re seeing that we have better tools for diagnosing everything, so consequently the prevalence of breast cancer is higher than it used to be and initially people were worried that was because our environment was completely polluted and there might be a role of that, but it also has to do with the fact that now we have MRI scanners that we didn’t have a generation ago that are very, very sensitive to detecting very small cancers. And so along with that increased prevalence of cancer is an improvement in its outcome because we now actually can diagnose some people who will not die from the disease. And the prevalence of prostate cancer is higher because it is recognized in so many men in whom it’s an asymptomatic condition that they would die from other causes and otherwise would never have been recognized in their lifetime. To a certain extent, I think the same is true of autism, that we have better tools. We have better diagnostic tools and so therefore the prevalence goes up, but also, hopefully, the prognosis improves because we’re increasingly able to have the sort of diagnostic precision to diagnose the milder or the borderline cases that maybe a generation ago may have just been written off as a peculiar child and now we can recognize, have a more specific condition that we can hopefully treat in a more thoughtful and considerate way.
Bookheimer: I think the availability of some interventions and some treatments makes it much more likely that people will want to get a diagnosis because then you have a place to go. But years ago when there were no available treatments and the diagnosis of autism was associated with a terrible outcome as well as terrible stigma—since many years ago it was thought to be due to parental behavior, which is of course untrue—then why would anyone want to diagnose their child with autism and why would any physician want to tell a parent that their child may have autism. So I think that the whole milieu socially has changed quite a bit to make it possible.
Fischbach: The first paper written on autism was in 1943. Autism existed way before 1943, but in terms of the stigma these children were called queer, idiots, schizoid, bizarre. No one had a name for them until one man, Leo Kanner in 1943 gathered a group of children and said there is something common about these children and it is a well defined entity, but the definition has just kept expanding since then.
***
Is Autism a Male Disorder?
Wilczynski: Only one out of five children with autism is female. Work by Dr. Simon Baron Cohen, at Cambridge, and others have said that the autistic brain is an "extreme male brain." What does that mean?
Walsh: I think at the root of your Wilczynski is how do we make sense of this degree to which males are affected so much more commonly than females. Is there a genetic underpinning for that? Is it an environmental one or does it have to do with differences in the male and the female brain? And again, I don’t think we know the answer yet. We originally looked for genetic causes maybe due to sex-linked genes, and that does not seem to obviously account for that large difference. And so that does begin to make you wonder whether there are some other differences between males and females, particularly maybe males just aren’t very good at social behavior to begin with and so they have a higher risk of autism on that basis. I certainly am here to say I represent at least one male who has much poorer social behavior than the woman, than my wife or my daughters. And so that might be along the lines of what he is suggesting or maybe some other potential answer to that.
Wilczynski: Conversely, as we’ve noted already there is no blood test to diagnose autism and so we find that there are also times where females are under diagnosed. A female who engages very infrequently socially is considered shy and so instead of being diagnosed at two or three she is not diagnosed at all or until she is much older and that is another area where we need diagnosticians to really be focusing.
Fischbach: There is no question there are differences between male and female brains. They are called sexual dimorphisms and you can point to different anatomical structures. The question is: is this related to the male hormone testosterone or are there other compensatory differences. And I think that is still undecided. But there are clear differences between and some- and there may be protective factors in a female brain. We just don’t know.
Bookheimer: I think that most of us wouldn’t believe that the main reason for the gender difference in autism is under diagnosis of girls. I think that it’s generally that case that there are many, many, many more cases of males with autism.
Wilczynski: Absolutely.
Fischbach: You know, at the high end of the spectrum, towards the Asperger’s side the ratio is 8 to 1 to 10 to 1. It’s really quite dramatic. The low end of the IQ spectrum it’s closer to 2 to 1 or 1 to 1, so there are really differences depending on what level of the severity of the disorder.
Walsh: That is an excellent point and it may be the that the high-functioning autism spectrum disorders lie Asperger’s and the low-functioning autism spectrum disorders where there is severe language and cognitive impairment may be very different conditions. And it may be that this male bias... has to do with that high functioning condition and that there might be a stronger genetic component to the lower-functioning cases.
Fischbach: For some reason girls may just compensate better and we just don’t understand. It would be wonderful if we did understand how they did that.
Walsh: That question of compensation may come as we understand the genetics better and we don’t know enough about the genetics yet to know, but as we understand more of the genetic risk factors then we can begin to ask the question: are there females that carry a genetic profile that should predispose them to autism but don’t get it, compared to males who have autism with a very similar sort of genetic risk profile. And so we hope to have the sort of tools to be able to ask those questions soon although we’re not quite there yet with the genetics.
***
How Can Autism Be Treated?
Wilczynski: What is the current state of treatment for autism? Anyone?
Bookheimer: There are many treatments for autism, but I think that we would agree that the most effective treatments are still behavioral treatments. There are some drug treatments, which perhaps Chris can tell us about. But behaviorally I think that most of us agree that early intense treatment is still the very best interventions for autism and usually involving increasing joint attention, getting children to learn how to attend together with their caregivers, involving parents in the care giving in the treatment process, and doing it intensely and as early as possible. Most people think that still gives us the best outcome in autism.
Wilczynski: Very good, and Chris, did you want to add to that?
Walsh: Yeah. I agree. The tried and true and the best documented methods of treatment involve this early behavioral intervention and it’s interesting that in animal models if you take a mouse and you do an enriched environment it changes patterns of gene expression in the brain. And so it will be interesting to see whether this kind of early behavioral intervention in humans may have actually some genetic or gene-expression profile in the human brain as well.
Fischbach: I bet it’s going to end up being a combination of behavioral therapy and some medicine. We just don’t know what the medicine is yet. It’s strange that we’re all saying genes point to synapses, to connections. But none of the traditional therapies used in other neuropsychiatric disorders that either increase or decrease the action of a certain transmitter at a synapse seem to be effective in autism, in the core symptoms of autism. They may help in reducing the anxiety component or the aggressive component, but the social cognition seems to be resistant to traditional synoptically active drugs. Something new is going to be needed here.
Bookheimer: I think in part that reflects a general problem in that we tend to want to find interventions, particularly pharmacal interventions that are going to treat autism as a whole when in fact I think that we’re going to end up being more successful in treating specific features of autism—the repetitive behaviors aspect of it, the anxiety aspect of it and so forth—rather than finding a single bullet, a magic pill that is going to do everything for us.
***
Will Autism Be Cured in Five Years?
Wilczynski: So tell us about what is going to happen over the next 5-to-10 years. Will there be a cure?
Bookheimer: I don’t think that there will be a cure in 5 to 10 years. I think that where we’re going is in more translational research in trying to find the pathways that lead us from genes to neurobiological differences that lead from neurobiological differences that we see for example in imaging with behavior and doing a better job of linking all of these pathways from the basic neuroscience all the way up through behaviors, so we at least can know how and where we can try to intervene in a way that is scientifically valid. But I don’t think that we’re going to find a cure for autism because I don’t think autism is really a single disorder and I think as long as that is the case we’re going to have to find many approaches to treating different aspects of autism and we need more basic science. We need more animal models.
Walsh: Yeah, I agree. I mean I think that on the one hand, this is a time of tremendous optimism. On the other hand we’re in a marathon, not a sprint and we just now have the first sort of beginning of what we hope will be a raging bonfire of possible treatments, but right now it’s just a couple of little hopeful flames that we’re trying to blow on and nurse as well as we can to get them going. But we feel like we have a small paradigm shift in sort of thinking about drugs that actually might change the way synapses work and it makes a lot of sense that they might be tremendously powerful, but we’ve got to be very, very cautious and really keep ourselves from getting sort of overly hopeful and overly confident that there is going to be cures anytime soon, but we do hope there is going to be better treatments.
Wilczynski: Very good.
Fischbach: I absolutely agree with both what Susan and Chris said. I think the word cure gets in the way. I don’t know of any neuropsychiatric disorder other than an infection that has been cured. But the goal is to improve the quality of life of people who experience autistic symptomology and I just think we will make progress on that. I think the behavioral therapy is a good clue and I think a lot of it will be empirical.
***
Aging With Autism
Wilczynski: We know that the many children who are diagnosed with autism today will become adults, in fact, about 500,000 of them in this decade. As you mentioned earlier the first child that was diagnosed with autism is now 77 years old, living a long life, and so what have we learned over this period of time?
Fischbach: Well we’ve learned that you really... that autism is not a snapshot. It’s a life. You really... I think many people have been interested in trajectories and I don’t... I'm not the expert in that area, but I think that things don’t dramatically get better. In a few people they do improve. Donald T., in the Atlantic article, was out in a community independent. But some people don’t. Some people deteriorate and require institutionalization. So I just think we have to... much more attention ought to be devoted to trajectories over time, so we get a better understanding of it.
Wilczynski: Even in the domain of behavioral treatments the vast majority of the research is for individuals who are three through early teen years. In fact, most of it is focused on even younger, the three to five year old range, but there is actually some pretty impressive data through the early teen years, but as we start approaching the 20s and into adulthood even among the treatments that have been shown to be effective very few researchers have been extending that work for that group. And absolutely the likelihood that individuals with autism will participate fully in their community will be directly related to our ability to serve them properly, so treatment, understanding the trajectory and then the treatment that is appropriate given that trajectory is really essential.
Fischbach: I think what many people have said today is that the brain compensates and sometimes the compensations are as difficult as the initial disorder, so it really means understanding the plasticity of the brain and what has happened that might be reversible in some of those.