Caregiving Takes Two Hands: High Touch & High Tech

Let me start by saying that I love this month’s Atlantic cover story, “The New Science of Old Age.” I’m not raising it up just to knock it down. The piece, by Gregg Easterbrook, adroitly addresses an issue that needs far more attention—the promise of biotech research to lengthen our lives. It also touches on a number of my personal obsessions: As lives extend, the need for our educational system to teach midlife-and-older adults new tricks. The demand for new, innovative financial products such as bank loans for older entrepreneurs. Above all, the fact that it will be essential to extend the healthy years of life as lifespans lengthen—the difference between added years of activity and infirmity.
Once more, I agree with 90 percent of what’s said in the article, which I encourage everyone to read. But there is one major point on which we differ: technologies for the care of older adults. Mr. Easterbrook writes: “With Japan at the leading edge of lengthening life expectancy, its interest in robotics can be eerie… A future in which large numbers of very old, incapacitated people stare into the distance as robot attendants click and hum would be a bad science-fiction movie if it didn’t stand a serious chance of happening.”
First, let’s recognize that he’s writing less about the threatof technology gone haywire than the consequences of what will happen if we don’t, as a society, get our act together in all sectors related to disruptive aging: funding caregiving jobs; investing in research for Alzheimer’s and other forms of dementia; and—above all—finding ways to expand our health span.
But still, the idea of robots caring for our most vulnerable feels understandably wrong to Easterbrook, as it does to many.
I don’t see it that way, because I reject the notion that we’re looking at an either-or: either we come up with enough skilled human caregivers (or somehow engineer it so that our oldest-old are healthy enough not to need many of them), or consign our elders to a sci-fi dystopian existence. Rather, I believe that there’s a right way to incorporate robotics and AI into how we age: simultaneously making the frailest years of life better for the very old, forestalling the onset of dependency for as long as possible, and helping caregivers. Remember, the vast majority of care that is provided to older adults happens in informal, not institutional, settings. Typically (and unfairly), the bulk of this labor of love often falls on the oldest adult daughter of the care recipient. Technologies that help such people cope with the stress, expense, and uncertainty of caregiving are to be embraced, not feared.
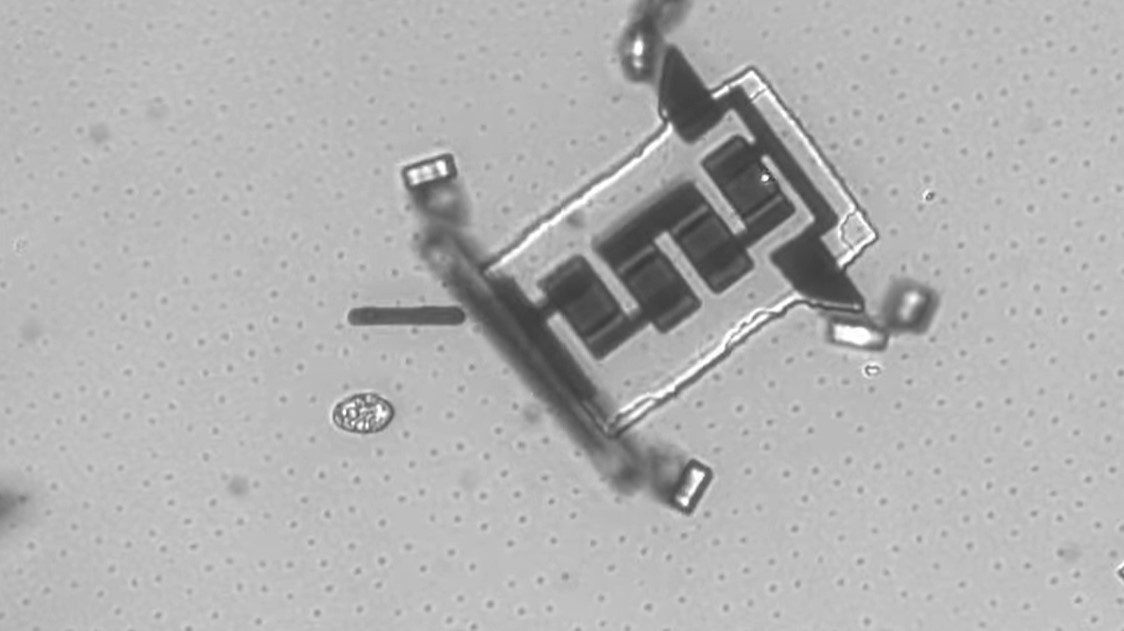
But even for those in institutional settings, robotics may hold more promise than peril. Consider those with severe dementia or Alzheimer’s, one of the gravest potential issues of a future in which longevity increases but the health span remains the same. At the AgeLab, we have two furry, snow-white baby seals named PARO that can improve life for such patients. PAROs 1 and 2 are robots that use a combination of tactile, light, audition, temperature, and posture sensors to interact with people with dementia in many of the ways that a pet would. But unlike a pet, PARO requires no upkeep or responsibility, which means people with serious cognitive issues can have and handle them. The moment someone with very severe dementia holds PARO for the first time and her eyes light up because she realizes here is a wonderful creature that I can care for,the effect isn’t dystopian. It’s a godsend, and better yet, PARO has been anecdotally observed to reduce “sundowning”—a common tendency in Alzheimer’s patients to become restless in the afternoon.
PARO is already seeing frequent use in many Japanese and European elder-care facilities. Robots in such settings by no means need to come across as cold automatons, and there’s no reason to assume that the next generations of such devices will do so. But despite the potential for technology to improve the nursing home experience, the devices most likely to affect the living of old age in the near future will be designed for those who hope to continue living independently. These technologies will include in-home sensors that can register falls or alert relatives to changes in an older adult’s daily routine. One such sensor, pioneered by IBM, tracks carbon dioxide emitted during cooking to determine whether meals are taking place regularly. If such measures seem like an invasion of privacy, consider that there is very little privacy in a nursing home. Any technology that keeps an older adult in her own home and not in an institutional setting effectively increases privacy and independence.
Looking farther down the road, another class of people who stand to benefit from robotics will be those who are fully mentally competent, but need help with physical, bodily issues. We all have different personalities, and some of us are less comfortable than others with the idea of human caregivers helping us in our most private moments. The option to choose between human or robotic care during such vulnerable instances may well provide older adults with more dignity, not less.
Ultimately, how technology is applied to the challenge of an older society will be up to the people involved. In the future, will it be used to improve on today’s level of care, or will it be used to cut budgetary corners? The first scenario will require a continued societal commitment to the wellbeing of older adults. That may not be so unlikely if, as Easterbrook suggests, older adults retain outsize political sway in the decades to come. And meanwhile, I’ve had many encounters with many in their 60s and 70s who work tirelessly to help those in their 80s and 90s. We need such a pay-it-forward ethos to catch on, especially in terms of investing in technology that makes old age better. To borrow a slogan, technology doesn’t care for people—people care for people, with technology.
And so we should keep an open mind toward technologies that can help an aging society, and a close eye on how they’re being used.
MIT AgeLab’s Luke Yoquinto contributed to this article.
Image: Shutterstock/Alexandra Ignatyeva